Basic Physical
Emotional Stability
Glutathione
DNA synthesis and repair
Protein synthesis
Amino acid transport
Enzyme catalysis
Enzyme activation
Metabolism of toxins
Metabolism of carcinogens
Metabolism of xenobiotics
Conjugation to heavy metals
Conjugation to xenobiotics
Enhancement of systemic immune function
Enhancement of humoral immune function
Resistance to UV radiation
Decreases radiation damage
Decreases free radical damage
Decreases oxyradical damage
Metabolizing of hydrogen peroxide (H2O2)
Recycling of other antioxidants (master antioxidant role)
Storage and transport of cysteine
Regulation of homocysteine
Participation in nutrient metabolism
Hydration
Hypoxia
Mental Clarity
pH Balance
The term pH is short for the potential of hydrogen. It is a measure of the acidity or alkalinity of our body’s fluids and tissues. It is measured on a scale from 0 to 14. The more acidic a solution is, the lower its pH. The more alkaline, the higher the number is.
A pH of 7 is perfectly neutral. The healthiest pH is one that is slightly alkaline. Optimally, we want a pH of 7.365. This number will fluctuate throughout the day, but the normal range is between 6 and 7.5.
Normally, the kidneys maintain our electrolyte levels, those of calcium, magnesium, potassium and sodium. When we are exposed to acidic substances, these electrolytes are used to combat acidity. High degrees of acidity force our bodies to rob minerals from the bones, cells, organs and tissues. Cells end up lacking enough minerals to properly dispose of waste or oxygenate completely. Vitamin absorption is compromised by mineral loss. Toxins and pathogens accumulate in the body and the immune system becomes suppressed.
How Can You Achieve a Proper pH?
Even though there are many sources of acidity and toxicity in our environments, the biggest contributor to unbalanced pH is our diet. Fruits and vegetables contain potassium, a natural buffer to acidity. The western diet contains little in the way of fresh and raw fruits and vegetables. Processed foods contain tons of sodium chloride-table salt-which constricts blood vessels and creates acidity. Eating too much animal protein causes sulfuric acid to build up in the blood as amino acids are broken down. All grains, whole or not, create acidity in the body. Americans ingest most of their plant food quota in the form of processed corn or wheat.
Our problem is more a matter of not taking in enough alkaline-promoting foods rather than taking in too much acid.
Calcium-rich dairy products cause some of the highest rates of osteoporosis. That’s because they create acidity in the body! When your blood stream becomes too acidic, it will steal calcium (a more alkaline substance) from the bones to try to balance out the pH level. So the best way to prevent osteoporosis is to eat lots of alkaline green leafy veggies!
Alkaline Foods including fruits, mushrooms and vegetables (especially citrus, dates, raisins and spinach) promote an alkaline pH. Strangely enough, acidic fruits such as grapefruit and tomatoes don’t create acidity in the body. They do just the opposite and contribute to an alkaline environment.
Raw foods-Uncooked fruits and vegetables are said to be biogenic or “life-giving.” Cooking foods depletes alkalinizing minerals. Increase your intake of raw foods, and try juicing or lightly steaming fruits and vegetables.
Alkaline water has a pH of 9 to 11. Distilled water is just fine to drink. Water filtered with a Reverse Osmosis filter is slightly acidic, but it’s still a far better option than tap water or purified bottled water. Adding pH drops, lemon or lime, or baking soda to your water boosts alkalinity.
Green Drinks-Drinks made from green vegetables and grasses in powder form are loaded with alkaline-forming foods and chlorophyll. Chlorophyll is structurally similar to our own blood and alkalizes the blood.
Vagal Tone



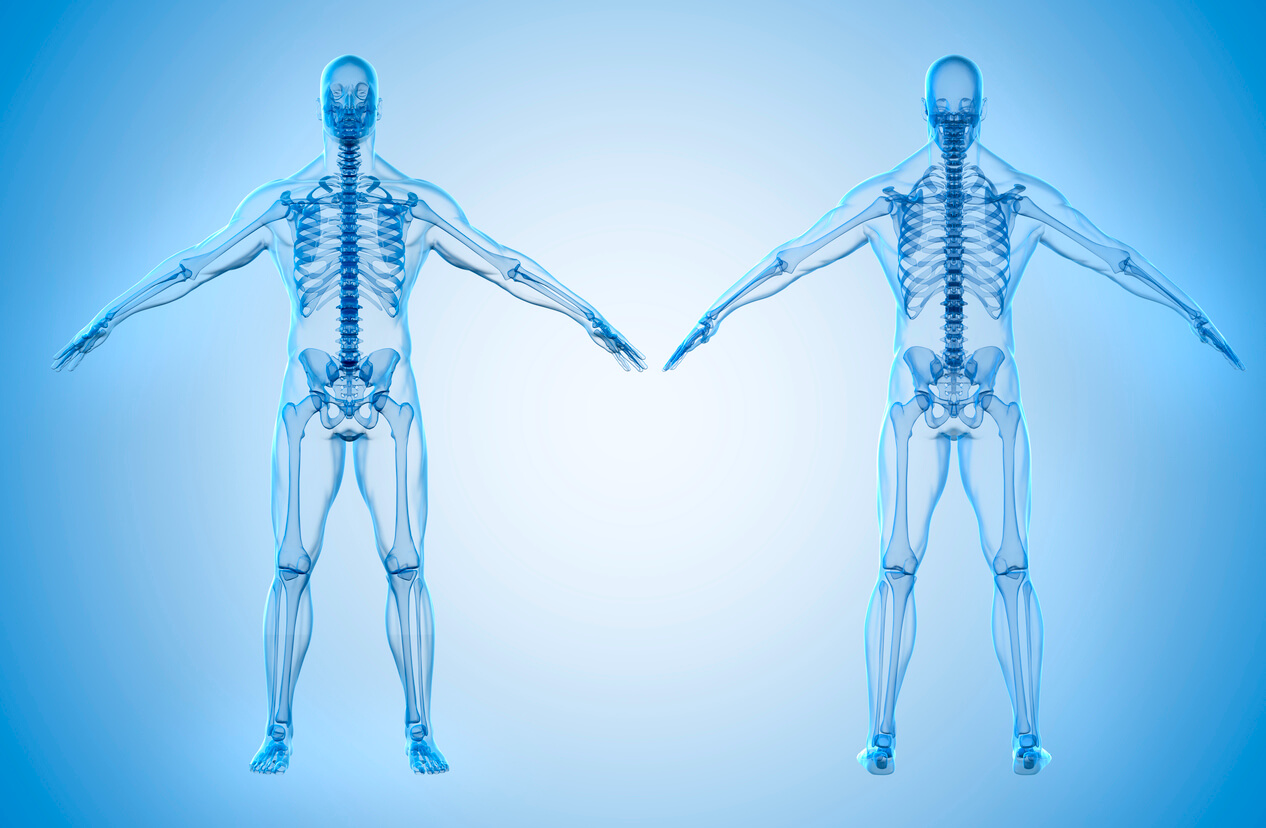
Bone and Muscle Condition
Adhesions of the Shoulder Muscles
The shoulder capsule thickens, swells, and tightens due to bands of scar tissue (adhesions) that have formed inside the capsule. As a result, there is less room in the joint for the humerus, making movement of the shoulder stiff and painful.
Age of Ligaments (Flexibility/Limberness)
This refers to the absolute range of movement in a joint or series of joints, and length in muscles that cross the joints to induce a bending movement or motion.
An increase in the level of fragmentation and dehydration
Changes in the chemical structure of the tissues.
Loss of suppleness due to the replacement of muscle fibers with fatty, collagenous fibers.
When connective tissue is overused, the tissue becomes fatigued and may tear, which also limits flexibility. When connective tissue is unused or under used, it provides significant resistance and limits flexibility. The elastin begins to fray and loses some of its elasticity, and the collagen increases in stiffness and in density. Aging has some of the same effects on connective tissue that lack of use has.
This does not mean that you should give up trying to achieve flexibility if you are old or inflexible. It just means that you need to work harder, and more carefully, for a longer period of time when attempting to increase flexibility. Increases in the ability of muscle tissues and connective tissues to elongate (stretch) can be achieved at any age.
Disc, Protrusion
This is a disease condition which can occur in some vertebrates, including humans, in which the outermost layers of the annulus fibrosus of the intervertebral discs of the spine are intact, but bulge when one or more of the discs are under pressure.
Disc, Degenerative
This is a condition of the discs between vertebrae with loss of cushioning, fragmentation and herniation related to aging. There may be no symptoms. In some cases, the spine loses flexibility and bone spurs may pinch a nerve root, causing pain or weakness.
Joints, Range of Motion
Range of motion (ROM) is a measurement of the distance and direction a joint can move to its full potential. A joint is a location in the body where bones connect. Most of them are constructed to allow movement in predetermined directions. Source
BOne & Growth Index
Bone Alkaline Phosphatase
Bone Healing (fracture healing)
This is a proliferative physiological process in which the body facilitates the repair of a bone fracture.Generally bone fracture treatment consists of a doctor reducing (pushing) displaced bones back into place via relocation with or without anesthetic, stabilizing their position to aid union, and then waiting for the bone’s natural healing process to occur.Adequate nutrient intake has been found to significantly affect the integrity of the fracture repair. Age, Bone type, drug therapy and pre existing bone pathology are factors which affect healing. The role of bone healing is to produce new bone without a scar as seen in other tissues which would be a structural weakness or deformity. Source
Cartilage Healing
Whether or not cartilage heals on its own depends on your age. Cartilage consists of collagen, the most abundant protein in the body. The collagen matrix of human cartilage becomes essentially permanent sometime in the teen years. After about age 15 or 16 there is no collagen regeneration in the cartilage. Your body, on its own, cannot regenerate the cartilage it loses in its adult years. However, in some cases, damaged cartilage will repair itself with tissue that is not the same; closer to a scar-like tissue. In other cases, the cartilage may heal with higher quality tissue. In any event, allowing healing to take place is better than not having it happen at all. Source
Epiphyseal Line
This is the part of the bone that replaces the epiphyseal growth plate in long bones once a person has reached their full adult height. Either rounded end of a long bone is called an epiphysis, and the shaft of the bone is called the diaphysis. The epiphyseal line is the marking that indicates where the two parts of the bone meet and where the epiphyseal plate was once located in children and young adults. An epiphyseal line is visible on a standard x-ray. It looks like a thin dark streak that stretches horizontally across the rounded ends of the bone. The line may be slightly raised and rougher than the surrounding bone. A person with abnormal bone growth may have a visible crack or an uneven line showing on an x-ray. Formation of this line takes place over many years. When the growth rate slows down after puberty, the cells stop the process of replication and all bone growth eventually stops. Ossification, the hardening of cells into bone, of the epiphyseal plate occurs when osteoblasts transform the cartilage cells found in the growth plate into bone. Once the entire growth plate is ossified, the epiphyseal line has formed. Source
Osteocalcin
This is the most abundant non-collagenous protein in bone, comprising almost 2% of total protein in the human body. It is important in bone metabolism and is used as a clinical marker for bone turnover, but its precise function remains elusive.
Source
Bone Mineral Density / Disease
Bone Hyperplasia
Bone Mineral Density
Calcification, Cervical
Calcification, Lumbar
Calcification, Sacrum
As people age, the ligaments of the spine can thicken and harden (called calcification). Bones and joints may also enlarge, and bone spurs (called osteophytes) may form. Bulging or herniated discs are also common. The sacroiliac joint connects the sacrum (the triangular bone at the bottom of the lumbar spine) on both sides to the pelvis’s ilium. The sacrum and the ilium are connected with a powerful network of ligaments.
The sacroiliac joint is highly susceptible to enthesitis and inflammation because it undergoes significant physical stresses and It has a relatively high concentration of fibrocartilage at the enthuses.
Sacroiliac joint inflammation can cause radiating pain that travels from the buttock to the thigh or lower back. Continued sacroiliitis and the inflammation-erosion-calcification cycle can eventually lead the bones of the sacroiliac joint to fuse together. While a normal sacroiliac joint has a minimal range of motion measured in just millimeters, sacroiliac joint fusion and immobility can cause pain as well as difficulty with bending forward, backward, and side-to-side.
Calcification, Thoracic
As people age, the ligaments of the spine can thicken and harden (called calcification). Bones and joints may also enlarge, and bone spurs (called osteophytes) may form. Bulging or herniated discs are also common. Spondylolisthesis (the slipping of one vertebra onto another) also occurs and leads to compression. Calcification of the thoracic region is referring to the area of the midback.
Calcium Loss
Calcium deficiency disease, also known as hypocalcemia, increases the risk of developing diseases like osteoporosis. Symptoms of hypocalcemia can include weak hair, nails, memory loss, and seizures.
Osteoclast Function
A type of bone cell that breaks down bone tissue. This function is critical in the maintenance, repair, and remodelling of bones of the vertebral skeleton. The osteoclast disassembles and digests the composite of hydrated protein and mineral at a molecular level by secreting acid and a collagenase, a process known as bone resorption. This process also helps regulate the level of blood calcium.
Osteoporosis
A medical condition in which the bones become brittle and fragile from loss of tissue, typically as a result of hormonal changes, or deficiency of calcium or vitamin D. The body constantly absorbs and replaces bone tissue. With osteoporosis, new bone creation doesn’t keep up with old bone removal.
Rheumatism (rheumatic disorder)
This is an umbrella term for conditions causing chronic, often intermittent pain affecting the joints and/or connective tissue. Any disease marked by inflammation and pain in thejoints, muscles, or fibrous tissue, especially rheumatoid arthritis. The term “rheumatism”, however, does not designate any specific disorder, but covers at least 200 different conditions.

Brain Nerve
Cerebral Arteriosclerosis
This is the result of thickening and hardening of the walls of the arteries in the brain. Symptoms of cerebral arteriosclerosis include headache, facial pain, and impaired vision. If the walls of an artery are too thick, or a blood clot becomes caught in the narrow passage, blood flow to the brain can become blocked and cause an ischemic stroke. When the thickening and hardening is uneven, arterial walls can develop bulges (called aneurysms). If a bulge ruptures, bleeding in the brain can cause a hemorrhagic stroke. Both types of stroke can be fatal.
Cerebral arteriosclerosis is also related to a condition known as vascular dementia, in which small, symptom-free strokes cause cumulative damage and death to neurons (nerve cells) in the brain. Personality changes in the elderly, such as apathy, weeping, transient befuddlement, or irritability, might indicate that cerebral arteriosclerosis is present in the brain. Computer tomography (CT) and magnetic resonance imaging (MRI) of the brain can help reveal the presence of cerebral arteriosclerosis before ischemic strokes, hemorrhagic strokes, or vascular dementia develop.
Cranial Nerves
Each cranial nerve is paired and is present on both sides. The numbering of the cranial nerves is based on the order in which they emerge from the brain, front to back (brainstem).
The terminal nerves, olfactory nerves (I) and optic nerves (II) emerge from the cerebrum or forebrain, and the remaining ten pairs arise from the brainstem, which is the lower part of the brain. The cranial nerves are considered components of the peripheral nervous system. However, on a structural level, the olfactory, optic, and terminal nerves are more accurately considered part of the central nervous system.
Cranial Nerve l, Olfactory
This nerve is instrumental for the sense of smell. It is one of the few nerves that are capable of regeneration.
Cranial Nerve II, Optic
This nerve carries visual information from the retina of the eye to the brain.
Cranial Nerve III, Oculomotor
This controls most of the eye’s movements, the constriction of the pupil, and maintains an open eyelid.
Cranial Nerve IV, Trochlear
A motor nerve that innervates the superior oblique muscle of the eye, which controls rotational movement.
Cranial Nerve V, Trigeminal
This is responsible for sensation and motor function in the face and mouth.
Cranial Nerve VI, Abducens
A motor nerve that innervates the lateral rectus muscle of the eye, which controls lateral movement.
Cranial Nerve VII, Facial
This controls the muscles of facial expression, and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue and oral cavity.
Cranial Nerve VIII, Vestibulocochlear
This is responsible for transmitting sound and equilibrium (balance) information from the inner ear to the brain.
Cranial Nerve IX, Glossopharyngeal
This nerve receives sensory information from the tonsils, the pharynx, the middle ear, and the rest of the tongue.
Cranial Nerve X, Vagus
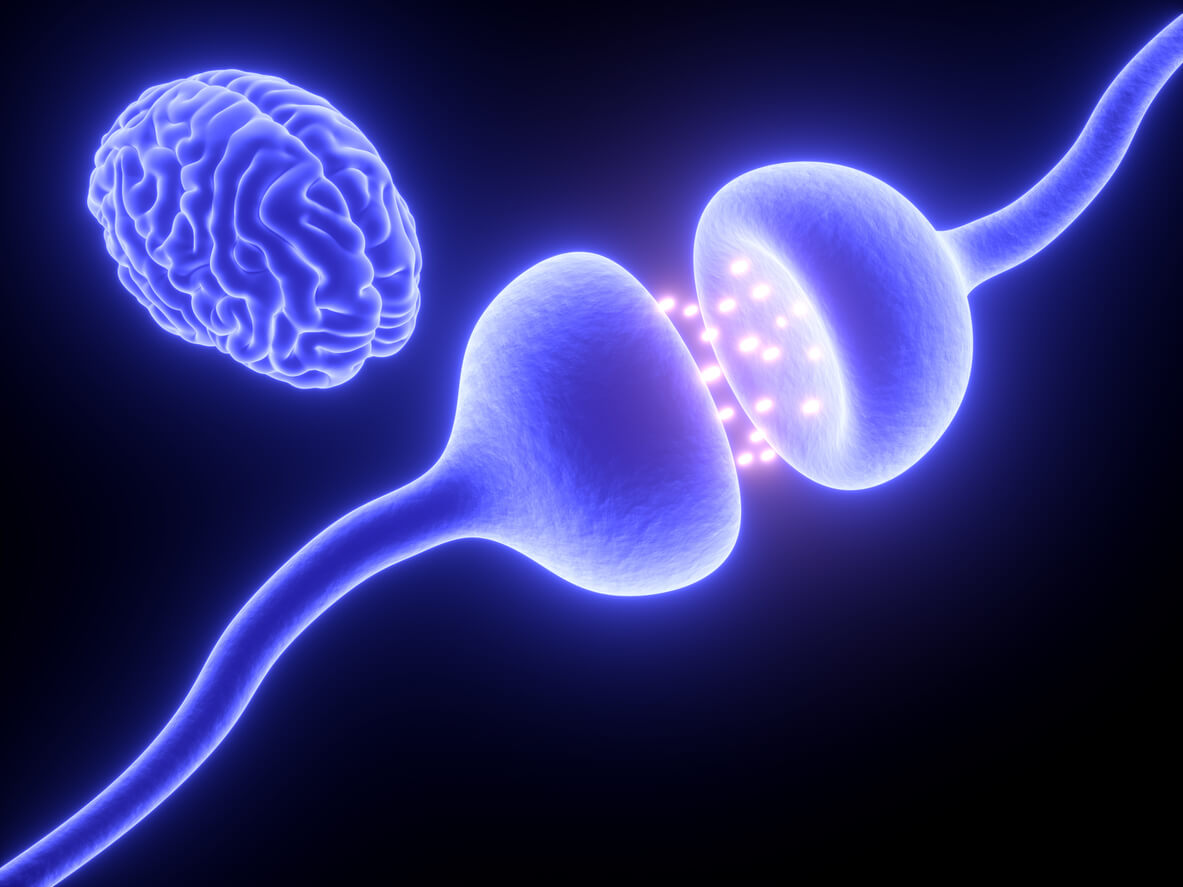
The vagus nerve can be thought of a superhighway that connects your body and your brain. It innervates most organs in the body; the messages zip along its five lanes of traffic with four lanes delivering information from the body to the brain and one lane moving information from the brain to the body. This is the most obvious physical representation of the mind-body connection. The vagus nerve both senses your internal environment (via its sensory neurons) and affects it (via its motor neurons).
Some of the functions of the vagus nerve have been long established, while others were discovered only recently.
Here is what we know about the vagus nerve so far:
1. It is intimately involved in managing sympathetic/parasympathetic balance in the autonomic nervous system (ANS). Here is a quick reminder how ANS works.
The vagus nerve provides 75% of all parasympathetic outflow. When the brain triggers parasympathetic activation, the vagus nerve carries the messages to the heart (decreasing the heart rate and blood pressure), to the lungs (to constrict the respiratory passageways), to every organ in the digestive system (to increase motility and blood flow to the digestive tract, to promote defecation), to the kidneys and bladder (to promote urination) and to reproductive organs (to aid in sexual arousal).
2. It communicates messages between the gut and the brain. 80% of the vagus nerve’s fibers (4 out of 5 traffic lanes) deliver information from the enteric nervous system (the second brain in the gut) to the brain.
3. It regulates the muscle movement necessary to keep you breathing. Your brain communicates with your diaphragm via the release of the neurotransmitter acetylcholine from the vagus nerve to keep you breathing. If the vagus nerve stops releasing acetylcholine, you will stop breathing.
4. It helps decrease inflammation. This occurs through the release of the neurotransmitter acetylcholine.
5. It has profound control over heart rate and blood pressure. For example, patients with heart failure, in which the heart fails to pump enough blood through the body, tend to have less active vagus nerves.
6. It helps improve your mood. Research shows that stimulation of the vagus nerve can be an effective treatment for chronic depression that has failed to respond to other treatments.
7. It is essential in fear management. Remember that “gut instinct” that tells you when something isn’t right? Turns out that the vagus nerve plays a major role in that. The signals from your gut get sent to the brain via the vagus nerve, and the signals from the brain travel back to the gut, forming a feedback loop. Healthy functioning of the vagus nerve helps us bounce back from stressful situations and overcome fear conditioning.
8. It plays a role in learning and memory. The vagus nerve facilitates learning and re-wiring, so to speak. New findings about the vagus nerve offer exciting possibilities for the treatment of post-traumatic stress disorder (PTSD). Stimulation of the vagus nerve might be able to speed up the process by which people with PTSD can learn to reassociate a non-threatening stimuli which triggers anxiety with a neutral and non-traumatic experience”. It can also help with healing sexual stress and trauma.
9. It can help relieve cluster headaches.
Cranial Nerve XI, Spinal Accessory
This nerve controls specific muscles of the shoulder and neck.
Cranial Nerve XII, Hypoglossal Nerve
This nerve controls the tongue movements of speech, food manipulation, and swallowing.
Memory Index (ZS)
This reflects the strength of a person’s memory. Cerebral arteriosclerosis, cerebral atrophy and others will lead to insufficient blood supply to the brain. The functional declination of hippocampal cells in the brain is the histological reason for memory decline in the elderly. Memory is divided into two kinds: one is auditory memory and visual memory.
Levels:
If the Memory Index readings are high this may indicate impaired short term memory.
If the Memory Index readings are low this may indicate impaired long term memory.
Parasymapthetic Nervous System Function
This (usually abbreviated PSNS, not PNS, to avoid confusion with the peripheral nervous system) is one of the three divisions of the autonomic nervous system, the others being the sympathetic nervous system and enteric nervous system. The autonomic nervous system is responsible for regulating the body’s unconscious actions. The parasympathetic system is responsible for stimulation of “rest-and-digest” or “feed and breed” activities that occur when the body is at rest, especially after eating, including sexual arousal, salivation, lacrimation (tears), urination, digestion and defecation. Its action is described as being complementary to that of the sympathetic nervous system, which is responsible for stimulating activities associated with the fight-or-flight response.
Nerve fibres of the parasympathetic nervous system arise from the central nervous system. Specific nerves include several cranial nerves, specifically the oculomotor nerve, facial nerve, glossopharyngeal nerve, and vagus nerve. Three spinal nerves in the sacrum (S2-4), commonly referred to as the pelvic splanchnic nerves, also act as parasympathetic nerves. Because of its location, the parasympathetic system is commonly referred to as having “craniosacral outflow”, which stands in contrast to the sympathetic nervous system, which is said to have “thoracolumbar outflow”.
Sympathetic Nervous System Function (SNS)
This is one of the two main divisions of the autonomic nervous system, the other being the parasympathetic nervous system (PSNS). The autonomic nervous system functions to regulate the body’s unconscious actions. The sympathetic nervous system’s primary process is to stimulate the body’s fight-or-flight response. It is, however, constantly active at a basic level to maintain homeostasis.
Cardiovascular / Cerebrovascular
Blood Fat
Blood Lipids (or blood fats) are lipids in the blood, either free or bound to other molecules. They are mostly transported in a protein capsule, and the density of the lipids and type of protein determines the fate of the particle and its influence on metabolism. The concentration of blood lipids depends on intake and excretion from the intestine, and uptake and secretion from cells. Blood lipids are mainly fatty acids and cholesterol. Hyperlipidemia is the presence of elevated or abnormal levels of lipids and /or lipoproteins in the blood, and is a major risk factor for cardiovascular disease.
Blood Viscosity
Blood viscosity is the thickness and stickiness of blood. It is a direct measure of the ability of blood to flow through the vessels. It is also a key screening test that measures how much friction the blood causes against the vessels, how hard the heart has to work to pump blood, and how much oxygen is delivered to organs and tissues. Importantly, high blood viscosity is easily modifiable with safe lifestyle-based interventions.
Brain Tissue Blood Supply Status
Brain Blood Supply; Blood transports oxygen and other nutrients necessary for the health of neurons, so a constant flow of blood to the brain must be maintained. According to Love and Webb, 1992, the brain uses approximately twenty percent of the body’s blood and needs twenty-five percent of the body’s oxygen supply to function optimally. Blood flow in a healthy person is 54 milliliters per 1000 grams of brain weight per minute. There are 740 milliliters of blood circulating in the brain every minute. 3.3 milliliters of oxygen are used per minute by every 1000 grams of brain tissue. This means that approximately 46 milliliters of oxygen are used by the entire brain in one minute. During sleep, blood flow to the brain is increased, but the rate of oxygen consumption remains the same.
Cerebral Blood Vessel Elasticity
Cerebral Blood Vessel Elasticity; Like a steel cylindrical pipe, an artery is comprised of an inner space (the “lumen”, filled with blood) enclosed by a wall. The wall is made up of a number of layers, two of which are muscle tissue and elastic tissue. When a region of the blood vessel wall weakens, it can balloon out to form a sac-like structure. This structure is called an aneurysm (a word derived from the Greek, aneurysma – widening), and the major problem associated with aneurysms is that they can rupture, an event, which may be fatal.
Cerebral Blood Vessel Resistance
Cerebrovascular Blood Oxygen Pressure (PaO2)
In the alveoli, the partial pressure of oxygen is around 100 mm Hg and that of carbon dioxide is around 40 mm Hg. In the cells of the body, the PaO2 is closer to 40. The range of normal for Pa02 is 75 – 100 mm Hg. If your Pa02 is less than this, it means you are not getting enough oxygen.
It is the differences in partial pressure between the capillaries and alveoli that drive oxygen from the alveoli into the capillaries in the lungs, and it is the difference between partial pressures of oxygen in the blood and that in the cells that drives the flow of oxygen from the tissue capillaries into cells. PaO2 is a measure of all the oxygen in the blood – both that which is attached to hemoglobin, and that which is dissolved in the plasma. The majority of oxygen is carried in the blood attached to hemoglobin and only around 1.5% is dissolved in plasma. A low-level of oxygen in the blood is referred to as hypoxemia. When hypoxemia results in a low level of oxygen in tissues it is then referred to as hypoxia. Tissue hypoxia results in tissue damage, and if not corrected, eventually cell death.
Cerebrovascular Blood Oxygen Saturation (Sa)
SaO2 is a measure of how much hemoglobin is occupied by oxygen.
Cerebrovascular Blood Oxygen Volume (CaCO2)
Cholesterol Crystal
Cholesterol Crystals, as cholesterol builds up along the wall of an artery, it crystallizes from a liquid to a solid state and then expands. When the cholesterol crystallizes, two things can happen. If it’s a big pool of cholesterol, it will expand, causing the “cap’ of the deposit to tear off in the arterial wall. Or the crystals, which are sharp needle-like structures, pole their way through the cap covering the cholesterol deposit. The crystals then work their way into the bloodstream. It is the presence of this material, as well as damage to an artery, that disrupts plaque and puts the body’s natural defense mechanism – clotting – into action, which can lead to dangerous, if not fatal clots. Cholesterol in moderation is healthy and necessary for life.
Coronary Artery Elasticity
Coronary Artery Elasticity is also referred to as arteriosclerosis, which is a group of diseases characterized by thickening and loss of elasticity of the arterial walls which progressively blocks the coronary arteries and their branches. Arteriosclerosis is the most common cause of cardiovascular disability and death. Other forms of arteriosclerosis include arteriolosclerosis and medialcalcific stenosis, both of which are uncommon in the coronary vasculature.
Coronary Artery Resistance
Coronary Perfusion Pressure
Coronary Perfusion Pressure; the heart is an aerobic organ that is dependent for its oxygen supply entirely on coronary perfusion. Under resting condition, the myocardium extracts the maximum amount of oxygen from the blood it receives. The O2 saturation of blood returning from the coronary sinus to the right atrium has the lowest saturation of any body organ (30%). Interruption of coronary blood flow will result in immediate ischemia. Coronary blood flow is directly dependent upon perfusion pressure and inversely proportional to the resistance of the coronary vessel. Coronary perfusion occurs in diastole hence diastolic pressure is more important than systolic pressure in determining coronary perfusion. Coronary vessels are divided into epicardial or conductance vessels (R1), pre capillary (R2) and microvascular vessels (R3). The epicardial vessels, the site most commonly affected by atherosclerosis, offer negligible resistance to coronary flow. Resistance to flow occurs in the pre capillary (R2), and microvascular (R3) vessels which are termed resistance vessels. The increase coronary blood flow in response to increase myocardial oxygen demand (MVO2) is achieved by the dilation of these resistance vessels. Three factors play a key role in modifying vascular tone; the accumulation of local metabolites, endothelial factors and neural tone. The accumulation of adenosine during ischemia is an example of local metabolic factors. The most important endothelial substance mediating vasodilation is nitric oxide (NO). Other important mediators are bradykinin, endothelium derived 2 hyperpolarizing factor, and prostacyclin. On the other hand, endothelin-1 (ET-1) is a well-known vasoconstricting substance. Angiotensin II and thromboxane A2 are other well-known endothelium derived constricting factors. Alpha-receptor adrenergic stimulation results in coronary vasoconstriction whereas beta 1 receptor stimulation leads to vasodilatation.
Galectin-3
This protein has been shown to be involved in the following biological processes: cell adhesion, cell activation and chemoattraction, cell growth and differentiation, cell cycle, and apoptosis. Given galectin-3’s broad biological functionality, it has been demonstrated to be involved in cancer, inflammation and fibrosis, heart disease, and stroke. have also shown that the expression of galectin-3 is implicated in a variety of processes associated with heart failure, including myofibroblast proliferation, fibrogenesis, tissue repair, inflammation, and ventricular remodeling. Galectin-3 associates with the primary cilium and modulates renal cyst growth in congenital polycystic kidney disease.
Total Peripheral Resistance(TPR)
Resistance to blood flow through arterioles and capillaries. the total resistance to flow of blood in the systemic circuit; the quotient produced by dividing the mean arterial pressure by the cardiac minute-volume.
Left Ventricular Effective Pump Power
The left ventricle is one of four chambers of the heart. It is located in the bottom left portion of the heart below the left atrium, separated by the mitral valve. The thickest of all the chambers, the left ventricle pumps oxygenated blood to tissues all over the body.
The left ventricle pumps oxygenated blood out to the Body to serve the vital needs of every cell of your Body. It pumps most effectively with a pronounced stretching of its’ muscular wall, which creates an optimal recoil effect (“Starlings’ Effect”). This generates the greatest force with each Ventricular Systole (the contraction of the heart ventricles) and the most effective emptying of the left ventricle.
It is very important for the health of your Left Ventricle to be physically active. The Heart is an Electro-Mechanical Pump. By staying active, you help to optimize the strength of the entire Heart musculature.
This also optimizes blood flow to all the cells of your body, which optimizes the function of all the internal organs, as well as your nervous system and sensoria. Sensorium (plural) are those parts of the brain that receive, process and interpret sensory stimuli.
A sensory stimulus is any event or object that is received by the senses and elicits a response from a person. The stimulus can come in many forms such as light, heat, sound, touch, as well as from internal factors. Source
Left Ventricular Ejection Impedance
This reflects the indicators of resistance status of the left ventricular outflow channel.
Influence Factors: (1) The fact whether the outflow channel has lesion. The aortic stenosis and other conditions can make VER increased. (2) The outflow channel has no lesion, while the emptying rate of aortic blood is slow, so VER is increased. (3) The entire vascular resistance is large.
Myocardial Blood Demand
The heart normally receives 4% of cardiac output, or ~ 250 mL/min of blood. Fatty acids and lactate are the predominant sources of energy, although glucose can be utilized. The myocardium cannot compensate for underperfusion by increasing oxygen extraction significantly (maximal ER is 90%), and thus the only compensatory mechanisms available are to increase blood flow by either changing regional vascular resistance or perfusion pressure.
There are two settings in which myocardial supply and demand can be mismatched – profoundly low perfusion pressures, and irreversible stenosis. In the latter setting, vasodilation of non-critically stenoses vessels can shunt blood away from fixed-diameter vessels, leading to a decrease in coronary blood flow to a susceptible region, a phenomena know as “coronary steal.”
Myocardial Blood Perfusion Volume
Myocardial Blood Perfusion is the damage to the heart and the risk of future heart damage.
Myocardial Oxygen Consumption
Myocardial Oxygen Balance is determined by the ratio of oxygen supply to oxygen demand. Increasing oxygen supply by increasing either arterial oxygen content or coronary blood flow leads to an increase in tissue oxygen levels (usually measured as the partial pressure of oxygen, pO2). Increasing oxygen demand alone (i.e. myocardial oxygen consumption) decreases tissue oxygen levels. Normally, when oxygen demand increases there is a proportionate increase in coronary blood flow and oxygen supply so that tissue oxygen levels are maintained during times of increased oxygen demand. This increase in blood flow is performed by local regulatory mechanisms. This tight coupling between oxygen demand and coronary blood flow is impaired in coronary artery disease because oxygen supply is limited by vascular stenosis.
NT-proBNP
BNP and NT-proBNP are substances that are produced in the heart and released when the heart is stretched and working hard to pump blood. Heart failure can be confused with other conditions, and it may co-exist with them. BNP and NT-proBNP levels can help doctors differentiate between heart failure and other problems, such as lung disease. An accurate diagnosis is important because the treatments are often different and must be started as soon as possible. Higher-than-normal results suggest that a person has some degree of heart failure, and the level of BNP or NT-proBNP in the blood is related to its severity. Although BNP and NT-proBNP are usually used to recognize heart failure, an increased level in people with acute coronary syndrome (ACS) indicates an increased risk of recurrent events.
Pulse Wave Velocity Coefficient
Arterial stiffness can be assessed noninvasively with the use of pulse wave velocity (PWV) measurement, that is, the velocity of the pulse wave to travel a given distance between 2 sites of the arterial system. Aortic PWV determined from a single measurement is strongly associated with the presence and extent of atherosclerosis and that this measurement is highly related to cardiovascular risk as assessed by the standard Framingham equations.
Stroke Index
A cardiodynamic measure. Stroke volume is the amount of blood the left ventricle ejects in one beat, measured in milliliters per beat (ml/beat). The stroke volume can be indexed to a patient’s body size by dividing by the body surface area to yield the stroke index.
Stroke Volume (SV) (Cardiac Stroke Volume)
This is the amount of blood pumped by the left ventricle of the heart in one contraction. The stroke volume is not all of the blood contained in the left ventricle. The heart does not pump all the blood out of the ventricle. Normally, only about two-thirds of the blood in the ventricle is put out with each beat. What blood is actually pumped from the left ventricle is the stroke volume and it, together with the heart rate, determines the cardiac output, the output of blood by the heart per minute. Stroke volume is an important determinant of cardiac output, which is the product of stroke volume and heart rate. Because stroke volume decreases in certain conditions and disease states, stroke volume itself correlates with cardiac function. Assessment of the cardiac output is important in determining the work that the heart is actually performing with respect to the rest of the cardiovascular system.
Vascular Elasticity
To understand Blood Vessel Elasticity, we first need to understand the anatomy of the vessels. There are three types of vessels – arteries, veins, and capillaries. Arteries, veins, and capillaries are not anatomically the same. They are not just tubes through which blood flows. Both arteries and veins have layers of smooth muscle surrounding them. Arteries have a much thicker layer, and many more elastic fibers as well. The largest artery, the aorta leaving the heart, also has cardiac muscle fibers in its walls for the first few inches of its length immediately leaving the heart. Arteries have to expand to accept the blood being forced into them from the heart, and then squeeze this blood into the veins when the heart relaxes. Arteries have the property of elasticity, meaning that they can expand to accept a volume of blood, then contract and squeeze back to their original size after the pressure is released. A good way to think of them is like a balloon. When you blow into the balloon, it inflates to hold the air. When you release the opening, the balloon squeezes the air back out. It is the elasticity of the arteries that maintains the pressure on the blood when the heart relaxes, and keeps it flowing forward. If the arteries did not have this property, your blood pressure would be more like 120/0, instead of 120/80 that is more normal. Arteries branch into arterioles as they get smaller. Arterioles eventually become capillaries, which are very thin and branching.
Vascular Resistance
Total Peripheral Resistance (TPR) is the sum of the resistance of all peripheral vasculature in the systemic circulation. This should not be confused with Pulmonary Vascular Resistance, which is the resistance in the pulmonary circulation. Vascular resistance is a term used to define the resistance to flow that must be overcome to push blood through the circulatory system. The resistance offered by the peripheral circulation is known as the systemic vascular resistance (SVR), while the resistance offered by the vasculature of the lungs is known as the pulmonary vascular resistance (PVR). The systemic vascular resistance may also be referred to as the total peripheral resistance. Vasoconstriction (i.e., decrease in blood vessel diameter) increases SVR, whereas vasodilation (increase in diameter) decreases SVR.

Collagen Index
Collagen occurs in many places throughout the body. Over 90% of the collagen in the human body, however, is type I.
The five most common types are:
Type I: skin, tendon, vascular ligature, organs, bone (main component of the organic part of bone)
Type II: cartilage (main collagenous component of cartilage)
Type III: reticulate (main component of reticular fibers), commonly found alongside type I
Type IV: forms basal lamina, the epithelium-secreted layer of the basement membrane
Type V: cell surfaces, hair and placenta
Synthesis of collagen requires vitamin C as a cofactor. A long-term deficiency in this vitamin results in impaired collagen synthesis and scurvy. Hydroxylation reactions are catalyzed by two different enzymes: prolyl-4-hydroxylase and lysyl-hydroxylase. Vitamin C also serves with them in inducing these reactions. In this service, one molecule of vitamin C is destroyed for each H replaced by OH. The synthesis of collagen occurs inside and outside of the cell. The formation of collagen which results in fibrillary collagen (most common form) is discussed here. Meshwork collagen, which is often involved in the formation of filtration systems, is the other form of collagen. All types of collagens are triple helices, and the differences lie in the make-up of the alpha peptides created in step 2.
The AO vitals scan looks at collagen in the following areas:
Bones
Cartilage
Eyes
Hair and Skin
Ligaments
Muscles
Nervous system
Organs
Teeth
Tendons
Vessels
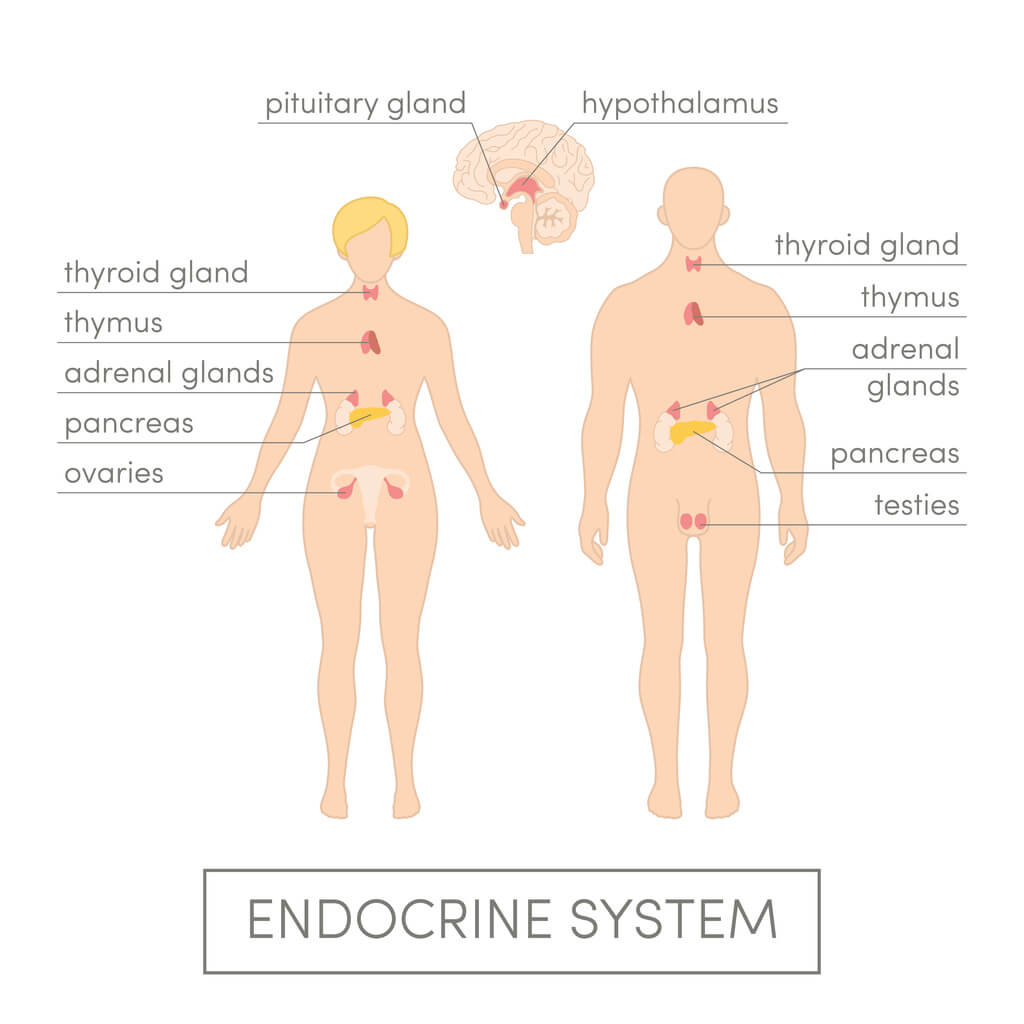
Endocrine Glands
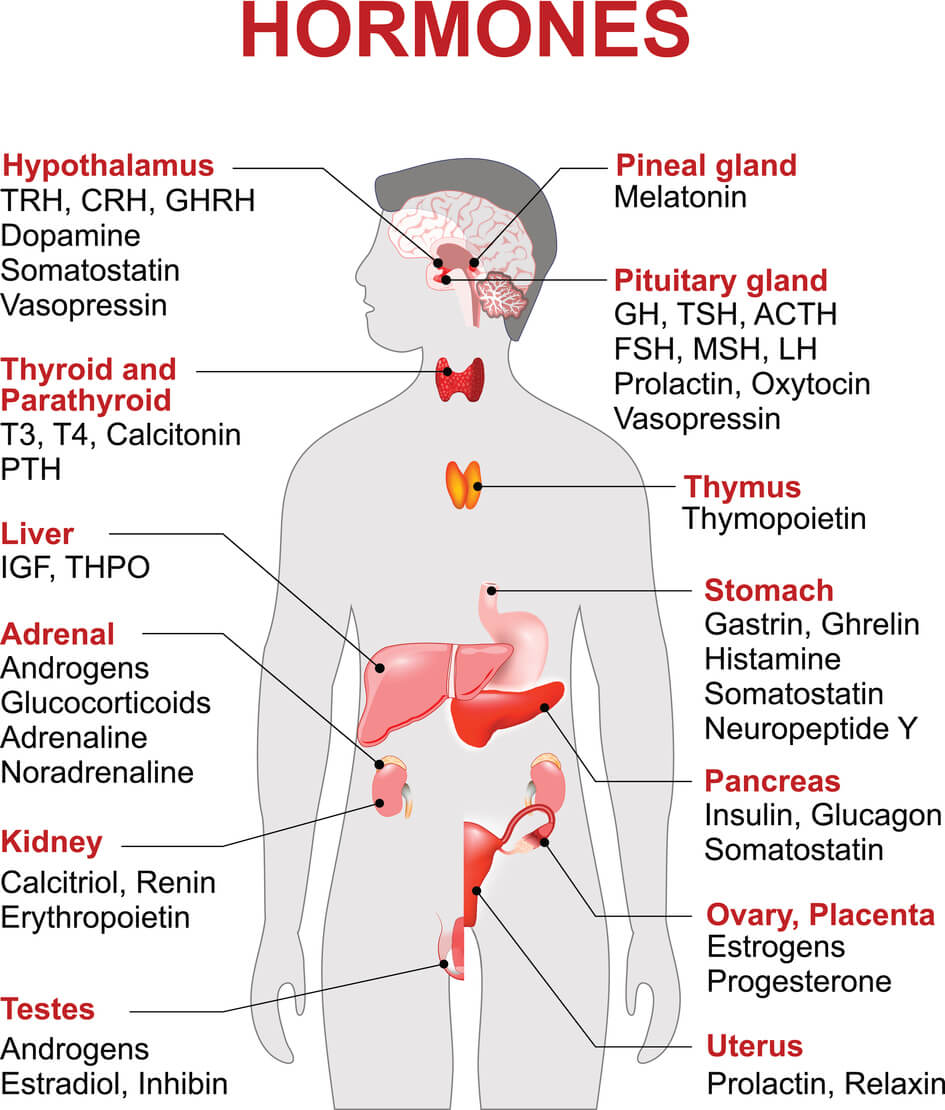
Adrenal Cortex
The outer portion of the adrenal gland located on top of each kidney. The adrenal cortex produces steroid hormones which regulate carbohydrate and fat metabolism and mineralocorticoid hormones which regulate salt and water balance in the body.
Adrenal Medulla
Rather than releasing a neurotransmitter, the cells of the adrenal medulla secrete hormones. The adrenal medulla consists of irregularly shaped cells grouped around blood vessels. These cells are intimately connected with the sympathetic division of the autonomic nervous system (ANS). In fact, these adrenal medullary cells are modified postganglionic neurons, and preganglionic autonomic nerve fibers lead to them directly from the central nervous system. The adrenal medulla therefore affects available energy, heart rate, and metabolism.
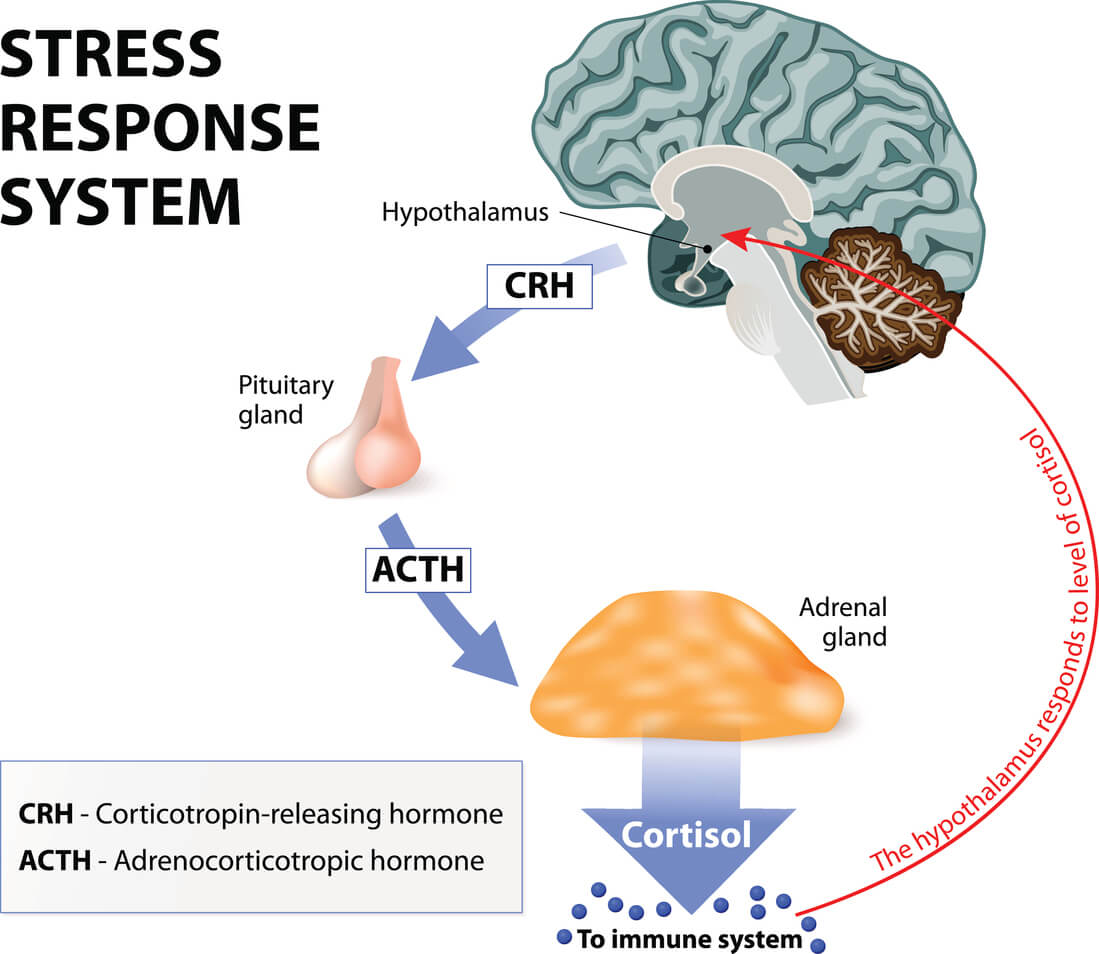
Hypothalamus
The hypothalamus (from Greek ὑπό, “under” and θάλαμος, thalamus) is a portion of the brain that contains a number of small nuclei with a variety of functions. One of the most important functions of the hypothalamus is to link the nervous system to the endocrine system via the pituitary gland (hypophysis).
The hypothalamus is located below the thalamus and is part of the limbic system. In the terminology of neuroanatomy, it forms the ventral part of the diencephalon. All vertebrate brains contain a hypothalamus. In humans, it is the size of an almond.
The hypothalamus is responsible for the regulation of certain metabolic processes and other activities of the autonomic nervous system. It synthesizes and secretes certain neurohormones, called releasing hormones or hypothalamic hormones, and these in turn stimulate or inhibit the secretion of pituitary hormones. The hypothalamus controls body temperature, hunger, important aspects of parenting and attachment behaviours, thirst, fatigue, sleep, and circadian rhythms. Source
Ovaries
These are organs found in the female reproductive system that produces an ovum. When released, this travels down the fallopian tube into the uterus, where it may become fertilised by a sperm. There is an ovary (from Latin ovarium, meaning egg/nut) found on the left and the right side of the body. The ovaries also secrete hormones that play a role in the menstrual cycle and fertility. The ovary progresses through many stages beginning in the prenatal period through menopause. It is also an endocrine gland because of the various hormones that it secretes. Source
Testes
The male sex gland, located behind the penis in a pouch of skin called the scrotum. The testes produce and store sperm and are also the body’s main source of male hormones, such as testosterone. These hormones control the development of the reproductive organs and other male characteristics, such as body and facial hair, low voice, and wide shoulders. Also, known as testicle.
Pancreas
It is a glandular organ in the digestive system and endocrine system of vertebrates. In humans, it is located in the abdominal cavity behind the stomach. It is an endocrine gland producing several important hormones, including insulin, glucagon, somatostatin, and pancreatic polypeptide, all of which circulate in the blood. The pancreas is also a digestive organ, secreting pancreatic juice containing bicarbonate to neutralize acidity of chyme moving in from the stomach, as well as digestive enzymes that assist digestion and absorption of nutrients in the small intestine. These enzymes help to further break down the carbohydrates, proteins, and lipids in the chyme. The pancreas is known as a mixed gland. Source
Parathyroid
They are small endocrine glands in the neck of humans and other tetrapods that produce parathyroid hormone. Humans usually have four parathyroid glands, variably located on the back of the thyroid gland. Parathyroid hormone and calcitonin (one of the hormones made by the thyroid gland) have key roles in regulating the amount of calcium in the blood and within the bones. Source
Pineal Body
The pineal gland, also known as the pineal body, conarium or epiphysis cerebri, is a small endocrine gland in the vertebrate brain. The pineal gland produces the hormone melatonin, a serotonin derived hormone which modulates sleep patterns in both circadian and seasonal cycles. Melatonin released into the blood and possibly also into the brain fluid, known as cerebrospinal fluid. The body’s daily (circadian) clock controls the production of pineal melatonin, so melatonin is commonly used in human research to understand the body’s biological time.
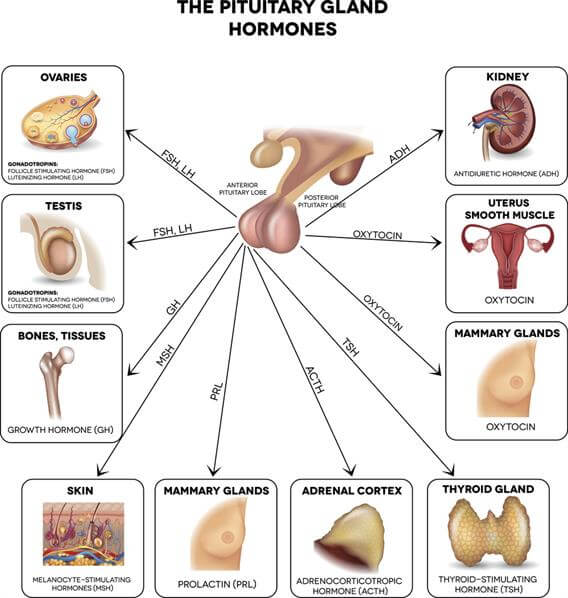
Pituitary, Anterior
The anterior pituitary contains five types of endocrine cell, and they are defined by the hormones they secrete: somatotropes (GH); prolactins (PRL); gonadotropes (LH and FSH); corticotropes (ACTH) and thyrotropes (TSH). Hormones secreted by the anterior pituitary are trophic hormones and tropic hormones. Trophic hormones directly affect growth either as hyperplasia or hypertrophy on the tissue it is stimulating. Tropic hormones are named for their ability to act directly on target tissues or other endocrine glands to release hormones, causing numerous cascading physiological responses. The anterior pituitary is the glandular, anterior lobe that together with the posterior lobe (posterior pituitary, or the neurohypophysis) makes up the pituitary gland.
Pituitary, Posterior
The posterior lobe of the pituitary gland which is part of the endocrine system. The posterior pituitary secretes the hormone oxytocin which increases uterine contractions and antidiuretic hormone (ADH) which increases reabsorption of water by the tubules of the kidney. Underproduction of ADH results in a disorder called diabetes insipidus characterized by inability to concentrate the urine and, consequently, excess urination leading potentially to dehydration. The urine is “insipid” (overly dilute).
Thyroid
Thyroid hormone (Triiodothyronine or T3) regulates our metabolic rate and is associated with modest changes in body weight and energy levels. it is an endocrine gland located in the front of our necks. It stores and produces hormones that affect the function of virtually every organ in our bodies. It plays a major role in the metabolism, growth and maturation of the human body. It helps to regulate many body functions by constantly releasing a steady amount of hormones into the bloodstream. More hormones are produced when the body needs more energy, like when it is growing or cold, or during pregnancy.
Uterus
The uterus has three layers: the inner lining (endometrium); the middle muscular layer (myometrium); and the outer layer (perimetrium). The uterus is connected to the fallopian tubes, the cervix, and (via the cervix) the vagina. The main purpose of the uterus is to nourish a fetus prior to birth.
Prostate
It is a compound tubuloalveolar exocrine gland of the male reproductive system in most mammals. Source
Eye Health
Bags Under the Eyes
Not getting enough sleep
Allergies or dermatitis, especially if puffiness is accompanied by redness and itching
Heredity – under-eye bags can run in families
Dark Circles
Some of the more common causes of dark circles under the eyes include:
Sleep deprivation is the most common cause, and the easiest to prevent, but …
Oversleeping can also cause dark eye circles.
Eczema
Stress
Age. As we get older, our skin becomes thinner.
Iron deficiency can prevent the blood from carrying sufficient oxygen to eye tissues.
Minor trauma that causes the appearance of a black eye.
Lifestyle. Excessive smoking or drinking can contribute to under-eye circles. Also, people who drink too much coffee or who use cocaine or amphetamines may have difficulty getting enough sleep.
Fluid retention, as may occur with pregnancy or weight gain.
Skin pigmentation abnormalities. The skin around the eyes is thinner, which is why your blood vessels are more readily visible through it.
Excessive exposure to the sun. Sun exposure encourages your body to produce more melanin.
Age. As we get older, we lose some of the fat and collagen surrounding our eyes. This loss, combined with the thinning of our skin, magnifies the appearance of dark eye circles.
Mononucleosis can cause the eyes to appear puffy and swollen. This is due partly to the fatigue that people feel when they are suffering from it, and partly because this illness causes a yellowing of the eyes and the skin around them (this is called jaundice).
Periorbital cellulitis. This is a bacterial infection of the eyelid or eyelids. If it is promptly treated with antibiotics, however, it is nothing to worry about.
Excess salt in the diet causes fluid retention throughout your body-including underneath your eyes.
Edema
Edema is swelling caused by excess fluid trapped in your body’s tissues. Edema is the medical term for swelling. Body parts swell from injury or inflammation. It can affect a small area or the entire body. Medications, infections, pregnancy, and many other medical problems can cause edema.
Edema happens when your small blood vessels become “leaky” and release fluid into nearby tissues. That extra fluid builds up, which makes the tissue swell.
Causes of edema things like a twisted ankle, a bee sting, or a skin infection will cause edema. In some cases, like an infection, this may be helpful. More fluid from your blood vessels puts more infection-fighting white blood cells in the swollen area. Even though edema affects all parts of your body, it’s most common on the hands, arms, feet, ankles and legs.
Eye Cell Activity
Lack of blood flow in the interior part of the eye makes it more vulnerable compared with other organs even in the case of weak thermal interactions. Protecting your eyes from winter elements like low temperatures, wind, and even the sun is essential to your ocular health.
Low body temperature causes dry eyes and other vision problems like blurred vision.
The cold can irritate your eyes and make them start to water. If it’s very cold, your eyelashes may freeze together. In severe conditions, your corneas can also freeze without the proper protection. Wind can predispose your eyes to pterygium growths. These are fleshy bumps that grow on the whites of your eyes like little calluses. They’re more common in people who spend time outdoors, so if you do a lot of skiing or other winter sports make sure you wear eye protection.
Reduced temperature will also slow the metabolism of cells and after a long period of time results in cell death.
Ultraviolet (UV) rays from the sun can damage your eyes in a number of ways, including contributing to cataracts and macular degeneration. High temperatures will also lead to eye cell death.
If your Eye Cell Activity reading is higher than 0.892, this may indicate a mild cellular reaction to abnormal body temperature. If you’re reading is higher than 1.37 this may indicate a moderate cellular condition to temperature and if you’re reading if higher than 1.892 this indicates a severe reaction to body temperature or eye temperature variance to normal. If your Eye Cell Activity reading is lower than 0.118, this is generally of no concern.
Lymphatic Obstruction
Also known as lymphedema is a condition that results from impaired flow of the lymphatic system. It’s an abnormal collection of high-protein fluid just beneath the skin. This swelling, or edema, occurs most commonly in the arm or leg, but it also may occur in other parts of the body including the breast or trunk, head and neck, or genitals. Lymphedema usually develops when lymph vessels are damaged or lymph nodes are removed (secondary lymphedema) but can also be present when lymphatic vessels are missing or impaired due to a hereditary condition (primary lymphedema).
Lymphatic fluid is normally transported out of a region of the body by an extensive network of lymph vessels. When the collection of protein-rich fluid persists in a specific area, it can attract more fluid and thus worsen the swelling. In addition to increased fluid in the area, the body experiences an inflammatory reaction resulting in scar tissue called fibrosis in the affected area. The presence of fibrosis makes it even more difficult for the excess fluid to be eliminated from the area. As a result, the increased fluid and fibrosis prevents the delivery of oxygen and essential nutrients to the area, which in turn can delay wound healing, provide a culture medium for bacteria to grow, and increase the risk of infections in or below the skin called cellulitis or lymphangitis.
Sagging
Skin sags with age primarily due to loss of volume in the underlying structures, such as soft tissue, fat and bone. The most common cause of sagging skin is aging. As you age, your skin loses its collagen and elastin in the dermis due to ultraviolet light., your skin’s supportive connective tissue, that make it look soft, plump and youthful. In addition, facial muscles can weaken with age, which takes a toll too. Getting older means more exposure to the dreaded pull of gravity; which we know causes skin to sag a little further down with each passing day.
Sun exposure is another reason for skin losing its elasticity. The sun’s powerful rays damage skin cells which, over time, this can increase the effects of aging.
Loss of large amounts of weight over a short period of time, can cause skin to sag. Those who undergo bariatric surgery often find themselves stuck with skin and tissue too stretched out to snap back.
Visual Fatigue
“Visual fatigue” provides a label for conditions experienced by individuals whose work involves extended visual concentration. It describes phenomena related to intensive use of the eyes. It can include complaints of eye or periocular pain, itching or burning, tearing, oculomotor changes, focal problems, performance degradation, “after colors,” and other phenomena. “Asthenopia,” another term for visual fatigue, is characterized by pain, discomfort, or fatigue in and around the eyes. The term in its current usage is equivalent to that of visual fatigue.
Visual fatigue results from visual inefficiencies or from eye-related symptoms caused by a combination of individual visual abnormalities and poor visual ergonomics. The problems (whether computer-related or not) occur whenever the visual demands of the task exceed the abilities of the individual. Symptoms of visual fatigue usually resolve with a combination of changes in the environment and appropriate visual care.
Information from these Sites:
http://www.mayoclinic.org/diseases-conditions/bags-under-eyes/basics/treatment/con-20034185)
http://www.eyehealthweb.com/dark-circles-under-eyes/)
http://www.webmd.com/heart-disease/heart-failure/edema-overview#1
http://diamarousa.com/eye-cell-activity/
http://www.lymphnet.org/le-faqs/what-is-lymphedema
http://health.howstuffworks.com/skin-care/problems/beauty/sagging-skin1.htm
http://www.mdguidelines.com/visual-fatigue


Hormones: Mood / Sex / Sleep / Stress
Cortisol
Cortisol is a steroid hormone, in the glucocorticoid class of hormones. When used as a medication, it is known as hydrocortisone. It is produced in humans by the zona fasciculata of the adrenal cortex within the adrenal gland. It is released in response to stress and low blood-glucose concentration. It functions to increase blood sugar through gluconeogenesis, to suppress the immune system, and to aid in the metabolism of fat, protein, and carbohydrates. It also decreases bone formation.
Dehydroepiandrosterone (DHEA)
Also, known as androstenolone, is an endogenous steroid hormone. It is the most abundant circulating steroid hormone in humans, in whom it is produced in the adrenal glands, the gonads, and the brain, where it functions predominantly as a metabolic intermediate in the biosynthesis of the androgen and estrogen sex steroids. However, DHEA also has a variety of potential biological effects in its own right, binding to an array of nuclear and cell surface receptors, and acting as a neurosteroid.
Epinephrine
Also, known as adrenalin or adrenaline, is a hormone, neurotransmitter and medication. Epinephrine is normally produced by both the adrenal glands and certain neurons. It plays an important role in the fight-or-flight response by increasing blood flow to muscles, output of the heart, pupil dilation, and blood sugar. it does this by its effects on alpha and beta receptors. It is found in many animals and someone cell organisms.
Estradiol (E2)
Estrogen
Estriol
Gonadotropin; are glycoprotein polypeptide hormones secreted by gonadotrope cells of the anterior pituitary of vertebrates. This family includes the mammalian hormones follicle-stimulating hormone (FSH), luteinizing hormone (LH), and placental/chorionic gonadotropins human chorionic gonadotropin (hCG) and equine chorionic gonadotropin (eCG), as well as at least two forms of fish gonadotropins. These hormones are central to the complex endocrine system that regulates normal growth, sexual development, and reproductive function. LH and FSH are secreted by the anterior pituitary gland, while hCG and eCG are secreted by the placenta in pregnant humans and mares, respectively. The gonadotropins act on the gonads, controlling gamete and sex hormone production.
Human Growth Hormone (HGH)
This is a peptide hormone that stimulates growth, cell reproduction, and cell regeneration in humans and other animals. It is thus important in human development. It is a type of mitogenwhich is specific only to certain kinds of cells. Growth hormone is a 191-amino acid, single-chain polypeptide that is synthesized, stored and secreted by somatotropic cellswithin the lateral wings of the anterior pituitary gland. Source
Human Sex Hormone-Binding Globulin
This is a glycoprotein that binds to the two sex hormones: androgen and estrogen. Source
Insulin-Like Growth Factor 1 (IGF-1)
This is a protein that in humans is encoded by the IGF1 gene. IGF-1 has also been referred to as a “sulfationfactor” and its effects were termed “nonsuppressible insulin-like activity” (NSILA) in the 1970s.
IGF-1 is a hormone similar in molecular structure to insulin. It plays an important role in childhood growth and continues to have anabolic effects in adults. A synthetic analog of IGF-1, mecasermin, is used for the treatment of growth failure.
IGF-1 consists of 70 amino acids in a single chain with three intramolecular disulfide bridges. IGF-1 has a molecular weight of 7,649 Daltons. Source
Luteinizing Hormone (LH)
Luteinizing hormone (LH) is produced and released in the anterior pituitary gland. This hormone is considered a gonadotrophic hormone because of its role in controlling the function of ovaries in females and testes in males, which are known as the gonads. Source
Melatonin
Norepinephrine
Progesterone
This is a steroid sex hormone that is the principal progestational agent; it plays a major part in the menstrual cycle. During the maturation of the secondary oocyte (ovum), estrogen, the principal female sex hormone, is produced at a high rate. At ovulation estrogen production is sharply reduced, and the ovary then creates within itself a special endocrine structure called the corpus luteum whose sole function is to produce progesterone. Unless fertilization takes place, the corpus luteum disappears when it has performed its function. The progesterone it has produced is promptly carried by the blood to the uterus, as was the estrogen previously. Both hormones now work to prepare the uterus for possible conception. In pregnancy progesterone acts in a way that protects the embryo and fosters growth of the placenta. By decreasing the frequency of uterine contractions it helps to prevent expulsion of the implanted zygote. It also promotes secretory changes in the mucosa of the fallopian tubes, thereby helping to provide nutrition for the fertilized ovum as it travels through the tube on its way to the uterus.
Prolactin
Prolactin is a hormone whose primary function is helping women produce milk after childbirth. It produced and secreted into the bloodstream by the anterior pituitary gland. Prolactin stimulates the development and growth of the mammary glands after the glands have been prepared by estrogen, progesterone, thyroxine, insulin, growth hormone, glucocorticoids, and human placental lactogen. After parturition, prolactin, together with glucocorticoids, is essential for the initiation and maintenance of milk production. Prolactin synthesis and release from the pituitary are mediated by the central nervous system in response to suckling by the infant. When suckling or its mechanical equivalent ceases, prolactin secretion slows and milk production ceases. Prolactin has no known function in human males.
Serotonin
Serotonin impacts every part of your body, from your emotions to your motor skills. Serotonin is considered a natural mood stabilizer and the chemical that helps sleeping, eating, and digesting. Serotonin also helps reduce depression, regulate anxiety, heal wounds, stimulate nausea, and maintain bone health. Serotonin is part of the reason why you become nauseous. Production of serotonin rises to push out noxious or upsetting food quicker in diarrhea. The chemical also increases in the blood, which stimulates the part of the brain that controls nausea. This chemical is responsible for stimulating the parts of the brain that control sleep and waking.
Testosterone
Testosterone is produced in the ovaries in women, the testes in men, and the adrenal glands in both genders. It is an androgen, or a hormone that stimulates the development of male characteristics. While men have it in higher amounts, men and women have testosterone to some extent. Testosterone is the hormone that initiates the internal and external development of a male fetus, including the reproductive organs. It plays an important role during male puberty, sparking growth spurts, hair growth and genital changes.
Testosterone-Free
Most of the testosterone in your blood attaches to two proteins: albumin and sex hormone binding globulin (SHBG). Free Testosterone is a test that measures the amount of unattached, or “free,” testosterone in your blood.
Immune System
Adenoids and Tonsils
Adenoids are made of similar tissue and are part of the immune system. Like tonsils, adenoids help to defend the body from infection. They trap bacteria and viruses which you breathe in through your nose. They contain cells and antibodies of the immune system to help prevent throat and lung infections.
Appendix
The appendix is near the junction of the small intestine and the large intestine and has abundant infection-fighting lymphoid cells, which suggests it plays a role in the immune system. Normally, the appendix sits in the lower right abdomen, but the actual function of the appendix is unknown.
Bone Marrow
Bone marrow is the spongy tissue inside some of your bones. It contains stem cells. The stem cells can develop into the red blood cells that carry oxygen through your body, the white blood cells that fight infections, and the platelets that help with blood clotting.
Immunoglobulin A (IgA)
An immunoglobulin test measures the level of certain immunoglobulins, or antibodies, in the blood. Antibodies are proteins made by the immune system to fight antigens, such as bacteria, viruses, and toxins. Selective IgA Deficiency is one of the most common primary immunodeficiency diseases. as many as one in every 500 Caucasian people has Selective IgA Deficiency. it is not understood why some individuals with IgA deficiency have almost no illness while others are very sick. A common problem in Selective IgA Deficiency is susceptibility to infections. This is seen in about half of the patients with IgA deficiency that come to medical attention. Recurrent ear infections, sinusitis, bronchitis and pneumonia are the most common infections seen in patients with Selective IgA Deficiency. A second major problem in IgA deficiency is the occurrence of autoimmune diseases. These are found in about 25% to 33% of patients who seek medical help. In autoimmune diseases, individuals produce antibodies or T-lymphocytes, which react with their own tissues with resulting inflammation and damage. The diagnosis of Selective IgA Deficiency is usually suspected because of chronic or recurrent infections, autoimmune diseases, chronic diarrhea or some combination of these problems.
Immunoglobulin D (IgD)
This is a monomeric antibody isotype that is expressed in the plasma membranes of immature B-lymphocytes. IgD is also produced in a secreted form that is found in small amounts in blood serum. Secreted IgD is made up of two heavy chains of the delta class, and two light chains. IgD’s function is to signal the B cells to be activated. By being activated, they are ready to take part in the defense of the body in the immune system. During B-cell differentiation, IgM is the exclusive isotype expressed by immature B cells. IgD starts to be expressed when the B-cell exits the bone marrow to populate peripheral lymphoid tissues. When a B-cell reaches its mature state, it co-expresses both IgM and IgD.
Immunoglobulin E (IgE)
This is one of the five subclasses of antibodies. Antibodies are proteins made by the immune system that attack antigens, such as bacteria, viruses, and allergens. IgE antibodies are found in the lungs, skin, and mucous membranes. IgE’s main function is immunity to parasites such as helminths like Schistosoma mansoni, Trichinella spiralis, and Fasciola hepatica. IgE is utilized during immune defense against certain protozoan parasites such as Plasmodium falciparum. IgE food allergies cause the release of histamine, producing an immediate hypersensitivity reaction, in which symptoms appear within minutes or hours. Prick skin tests can be used to identify specific IgE sensitization.
Immunoglobulin G (IgG)
This is a type of antibody. Each IgG has two antigen binding sites. Representing approximately 75% of serum antibodies in humans, IgG is the most common type of antibody found in the circulation. IgG molecules are created and released by plasma B cells. Antibodies are major components of humoral immunity. IgG is the main type of antibody found in blood and extracellular fluid allowing it to control infection of body tissues. By binding many kinds of pathogens such as viruses, bacteria, and fungi, IgG protects the body from infection. IgG (immunoglobulin G) testing is a useful guide for structuring elimination diets in many chronic conditions. Individuals with neurological, gastrointestinal, and movement disorders often suffer from IgG food allergies. These people may continue to eat offending foods unaware of their potential effects.
THE BENEFITS OF TESTING
Helps determine if food reactions are contributing to physical or mental symptoms.
Removal of highly reactive foods from the diet is a non-invasive, food-based therapy that often mitigates a patient’s symptoms.
Research and clinical studies suggest food allergies identified by IgG testing can be a major contributing factor in many chronic health conditions.
Food rotation and elimination diets can reduce stress on the immune system, lower gut inflammation, resolve food cravings, and reduce the potential for eating disorders.
Immunoglobulin M (IgM)
This is a basic antibody that is produced by B cells. IgM is by far the physically largest antibody in the human circulatory system. It is the first antibody to appear in response to initial exposure to an antigen. IgM is a polymer, where multiple immunoglobulins are linked together by strong covalent bonds known as disulfide bonds.
Liver
The liver is a large, meaty organ that sits on the right side of the belly. The liver also detoxifies chemicals and metabolizes drugs. As it does so, the liver secretes bile that ends up back in the intestines. The liver also makes proteins important for blood clotting and other functions.
Lymph Nodes
Lymph nodes are small, bean-shaped glands throughout the body. They are part of the lymph system, which carries fluid (lymph fluid), nutrients, and waste material between the body tissues and the bloodstream. The lymph system is an important part of the immune system, the body’s defense system against disease.
Lymphatic Vessels (Lymph Vessels/Lymphatics)
These are thin-walled, valved structures that carry lymph. As part of the lymphatic system, lymph vessels are complementary to the cardiovascular system. Lymph vessels are lined by endothelial cells, and have a thin layer of smooth muscles, and adventitia that bind the lymph vessels to the surrounding tissue. Lymph vessels are devoted to propulsion of the lymph from the lymph capillaries, which are mainly concerned with absorption of interstitial fluid from the tissues. Lymphatic capillaries are designed to pick up the fluid that leaks into your tissues from your bloodstream and return it to your circulatory system.
Mucosa
This is a membrane that lines various cavities in the body and surrounds internal organs. It consists of one or more layers of epithelial cells overlying a layer of loose connective tissue. It is Having to do with a mucous membrane. For example, the oral mucosa.
Peyer’s Patches
They are organized lymphoid follicles, named after the 17th-century Swiss anatomist Johann Conrad Peyer. They are an important part of gut associated lymphoid tissue usually found in humans in the lowest portion of the small intestine. Because the lumen of the gastrointestinal tract is exposed to the external environment, much of it is populated with potentially pathogenic microorganisms. Peyer’s patches thus establish their importance in the immune surveillance of the intestinal lumen and in facilitating the generation of the immune response within the mucosa. Pathogenic microorganisms and other antigens entering the intestinal tract encounter macrophages, dendritic cells, B-lymphocytes, and T-lymphocytes found in Peyer’s patches and other sites of gut-associated lymphoid tissue (GALT). Peyer’s patches thus act for the gastrointestinal system much as the tonsils act for the respiratory system, trapping foreign particles, surveilling them, and destroying them.
Spleen
The spleen is the largest lymphatic organ in the body. The spleen also filters blood, serves as a major reservoir for blood, and destroys blood cells that are aged.
Thymus
The thymus, despite containing glandular tissue and producing several hormones, is much more closely associated with the immune system than with the endocrine system. The thymus serves a vital role in the training and development of T-lymphocytes or T cells, an extremely important type of white blood cell. T cells defend the body from potentially deadly pathogens such as bacteria, viruses, and fungi. The function of the thymus is to receive immature T cells that are produced in the red bone marrow and train them into functional, mature T cells that attack only foreign cells. T cells first reside within the cortex of the thymus where they come in contact with epithelial cells presenting various antigens. The immature T cells that respond to the antigens corresponding to foreign cells are selected to survive, mature, and migrate to the medulla while the rest die via apoptosis and are cleaned up by macrophages. This process is known as positive selection.
Kidney Function
Blood Urea Nitrogen (BUN)
This is an indicator of kidney function. Urea is a metabolic byproduct which can build up if kidney function is impaired. The BUN-to-creatinine ratio generally provides more precise information about kidney function and its possible underlying cause compared with creatinine level alone. BUN also increases with dehydration.
Creatinine, Serum (mg/dL)
Creatinine has been found to be a fairly reliable indicator of kidney function. Elevated creatinine level signifies impaired kidney function or kidney disease. As the kidneys become impaired for any reason, the creatinine level in the blood will rise due to poor clearance of creatinine by the kidneys. Abnormally high levels of creatinine thus warn of possible malfunction or failure of the kidneys. It is for this reason that standard blood tests routinely check the amount of creatinine in the blood.
Cystatin C
This is used as a biomarker of kidney function. High levels indicate a decline in kidney function.
Proteinuria
Urine containing an abnormal amount of protein. The condition is often a sign of kidney disease. Healthy kidneys do not allow a significant amount of protein to pass through their filters. But filters damaged by kidney disease may let proteins such as albumin leak from the blood into the urine. The two most common risk factors for proteinuria are diabetes and high blood pressure.
Uric Acid
The uric acid blood test is used to detect high levels of this compound in the blood in order to help diagnose gout. The test is also used to monitor uric acid levels in people undergoing chemotherapy or radiation treatment for cancer. Rapid cell turnover from such treatment can result in an increased uric acid level. The uric acid urine test is used to help diagnose the cause of recurrent kidney stones and to monitor people with gout for stone formation.
Urobilinogen
This is a colourless by-product of bilirubin reduction. It is formed in the intestines by bacterial action on bilirubin. About half of the urobilinogen formed is reabsorbed and taken up via the portal vein to the liver, enters circulation and is excreted by the kidney. Low urine urobilinogen may result from complete obstructive jaundice or treatment with broad-spectrum antibiotics, which destroy the intestinal bacterial flora. (Obstruction of bilirubin passage into the gut or failure of urobilinogen production in the gut.) Low urine urobilinogen levels may result from congenital enzymatic jaundice (hyperbilirubinemia syndromes) or from treatment with drugs that acidify urine, such as ammonium chloride or ascorbic acid.Elevated levels may indicate hemolytic aneamia (excessive breakdown of red blood cells RBC), overburdening of the liver, increased urobilinogen production, re-absorption – a large hematoma, restricted liver function, hepatic infection, poisoning or liver cirrhosis.

Liver and Gall Bladder Function
ALP
ALT (Alanine Aminotransferase)
Moreover, the elevation of ALT activity persists longer than does AST activity. Elevated alanine aminotransferase (ALT) values are seen in parenchymal liver diseases characterized by a destruction of hepatocytes. Values are typically at least ten times above the normal range. Levels may reach values as high as one hundred times the upper reference limit, although twenty to fifty-fold elevations are most frequently encountered. In infectious hepatitis and other inflammatory conditions affecting the liver, ALT is characteristically as high as or higher than aspartate aminotransferase (AST), and the ALT/AST ratio, which normally and in other condition is <1, becomes greater than unity. ALT levels are usually elevated before clinical signs and symptoms of disease appear.
AST (Aspartate Aminotransferase)
A test measures the amount of this enzyme in the blood. AST is normally found in red blood cells, liver, heart, muscle tissue, pancreas, and kidneys. Low levels of AST are normally found in the blood. When body tissue or an organ such as the heart or liver is diseased or damaged, additional AST is released into the bloodstream. The amount of AST in the blood is directly related to the extent of the tissue damage. After severe damage, AST levels rise in 6 to 10 hours and remain high for about 4 days.
The AST test may be done at the same time as a test for alanine aminotransferase, or ALT. The ratio of AST to ALT sometimes can help determine whether the liver or another organ has been damaged. Both ALT and AST levels can test for liver damage.
An aspartate aminotransferase (AST) test is done to: Check for liver damage, Help identify liver disease, such as hepatitis (liver disease may produce symptoms such as pain in the upper abdomen, nausea, vomiting, and sometimes jaundice). Check on the success of treatment for liver disease, find out whether jaundice was caused by a blood disorder or liver disease, and keep track of the effects of medicines that can damage the liver.
Bile Secretion Function
Bile is a digestive juice that is secreted by the liver and stored in the gallbladder. Bile does not contain enzymes like other secretions from the gastrointestinal tract. Instead it has bile salts (acids) which can emulsify fat and break it down into small particles with its detergent-like action. And then help the body absorb these broken-down products of fat in the gut. Bile salts bind with lipids to form micelles. This is then absorbed through the intestinal mucosa. The other important function of bile is that it contains waste products from hemoglobin break down. This is known as bilirubin and is normally formed by the body as it gets rid of old red blood cells which are rich in hemoglobin. Bile also carries excess cholesterol out of the body and ‘dumps’ it into the gastrointestinal tract where it can be passed out with other waste matter.
The liver cells (hepatocytes) produce bile which collects and drains into the hepatic duct. From here it can enter the small intestine to act on fats by traveling down the common bile duct, or it can enter the gallbladder through the cystic duct, where it is stored.
The liver manufactures between 600ml to 1 liter of bile in a day. As bile travels down the ducts, the lining of these passages, secrete water, sodium and bicarbonate ions into the bile, thereby diluting it. These additional substances help to neutralize the stomach acid which enters the duodenum with partially digested food (chyme) from the stomach.
Bilirubin
A bilirubin test is used to detect an increased level in the blood. It may be used to help determine the cause of jaundice and/or help diagnose conditions such as liver disease, hemolytic anemia, and blockage of the bile ducts. Bilirubin is an orange-yellow pigment, a waste product primarily produced by the normal breakdown of heme. Heme is a component of hemoglobin, which is found in red blood cells (RBCs). Bilirubin is ultimately processed by the liver to allow its elimination from the body. Any condition that accelerates the breakdown of RBCs or affects the processing and elimination of bilirubin may cause an elevated blood level. Two forms of bilirubin can be measured or estimated by laboratory tests:
•Unconjugated bilirubin-when heme is released from hemoglobin, it is converted to unconjugated bilirubin. It is carried by proteins to the liver. Small amounts may be present in the blood.
•Conjugated bilirubin-formed in the liver when sugars are attached (conjugated) to bilirubin. It enters the bile and passes from the liver to the small intestines and is eventually eliminated in the stool. Normally, no conjugated bilirubin is present in the blood.
In adults and older children, bilirubin is measured to:
•Diagnose and/or monitor diseases of the liver and bile duct (e.g., cirrhosis, hepatitis, or gallstones).
•Evaluate people with sickle cell disease or other causes of hemolytic anemia; these people may have episodes called crises when excessive RBC destruction increases bilirubin levels.
In newborns with jaundice, bilirubin is used to distinguish the causes of jaundice.
•In both physiologic jaundice of the newborn and hemolytic disease of the newborn, only unconjugated (indirect) bilirubin is increased.
•In much less common cases, damage to the newborn’s liver from neonatal hepatitis and biliary atresia will increase conjugated (direct) bilirubin concentrations as well, often providing the first evidence that one of these less common conditions is present.
It is important that an elevated level of bilirubin in a newborn be identified and quickly treated because excessive unconjugated bilirubin damages developing brain cells. The consequences of this damage include mental retardation, and developmental disabilities, hearing loss, eye movement problems, and death.
Detoxification Function, Phase I
Your body doesn’t like to keep any molecules around for a long time. Even “good” molecules, such as hormones, are constantly being disassembled and reconstructed to prepare them to be recycled or eliminated. Thanks to detoxification enzymes, the liver is able to break up most molecules, even toxic and dangerous ones. Enzymes are molecules that act as catalysts in the transformation process. There are thousands of different enzymes, each with a unique role.
Think of this detoxification process as a two-phase wash cycle. Enzymes are like the soap that liberates grease into little droplets, removing impurities that the water can’t remove on its own.
In the first part of the wash cycle (Phase 1), enzymes break toxins down into intermediate forms. Some toxins are ready for elimination at this stage, but others require a second wash cycle. In Phase 2, these intermediate compounds are routed along one of six chemically driven detoxification pathways, where they are further broken down, and then bound to specific types of protein molecules which act as “escorts” to guide them out of the body, allowing them to exit through the kidneys (in the form of urine) or the bile (in the form of feces). This process is called conjugation.
When the liver is “sluggish,” Phase 1 of the detoxification cycle may not be processing toxins at a normal and necessary speed. This causes toxins to accumulate in the bloodstream. If the hormone estrogen, for example, is not dismantled during Phase 1, the buildup can reach potentially harmful levels. Premenstrual tension can be an expression of this. Many factors can cause Phase 1 to become sluggish. As we age, our detoxification processes slow. Use of medications such as anti-ulcer drugs (cimetidine) and oral contraceptives; exposure to cadmium, lead, and mercury; and consumption of large amounts of sugar and hydrogenated fats hinder Phase 1 detoxification.
Substances that slow down Phase 1 detoxification, setting the stage for a toxic buildup, are called Phase 1 inhibitors. They affect the DNA of the liver cells, causing less detoxification enzymes to be produced. In addition to those mentioned previously, Phase 1 inhibitors include:
• Grapefruit
• Turmeric
• Capsicum (found in hot peppers)
• Cloves
• Drugs containing benzodiazepenes and antidepressants
• Antihistamines
• Ketoconazole (used in antifungal medications)
• Toxins from bacteria in the intestines
A different type of detoxification problem develops if Phase 1 breaks down toxins at so fast a rate that Phase 2 cannot keep up. In this situation, the toxic intermediates produced during Phase 1 waiting to be washed out in Phase 2 flood the system. Many of these intermediate compounds-stuck in between Phase 1 and Phase 2-are more dangerous than the original toxin. This bottleneck can become a biochemical nightmare, damaging the liver, brain, and immune system.
Some of the substances that accelerate the breakdown of toxins in the liver by increasing the production of Phase 1 enzymes, without a concurrent increase in Phase 2 enzymes, are known carcinogens-pesticides, paint fumes, and cigarette smoke. Others are well known for their detrimental effects, such as alcohol and steroids. Even some otherwise harmless substances such as limonene from lemons, increase Phase 1 detoxification. But unlike cigarette smoke, limonene does not create dangerous intermediate molecules. As you read the following list, keep in mind that it is not strictly a list of “bad” things, but of those that increase the rate of Phase 1 detoxification, and that this becomes a problem only when Phase 2 can’t keep up.
• Phenobarbital
• Steroids
• Sulfonamide medications
• Foods in the cabbage family
• Charbroiled meats
• High-protein diets
• Citrus fruits
• Vitamin B1
• Vitamin B3
• Vitamin C
• Environmental toxins (exhaust fumes, paint fumes, dioxin, pesticides)
• Cigarette smoke
• Alcohol
• Endotoxins from intestinal bacteria in the bloodstream
Exposure to a toxin, when coupled with exposure to another substance that speeds up Phase 1, is especially dangerous. The combination of alcohol and acetaminophen provides a good example. It’s not uncommon to drink heavily, and later take acetaminophen for the headache that follows. The intermediate compound (from acetaminophen) is an extremely toxic substance called n-acetyl-p-benzoquinoneimine (NAPQI). Under normal conditions, NAPQI is removed quickly during Phase 2, but alcohol intake forces more NAPQI into the liver than Phase 2 can handle.
Research has shown that specific foods and nutrients not only have a beneficial effect on detoxification capability, but can also provide a safe and viable approach to treating a variety of immune disorders and toxicity syndromes.
If two or more detoxification accelerants are combined, they can interact, with serious consequences. An individual on a prescription medication who smokes, for example, actually needs higher dosages of the medication because smoking causes the medication to be broken down faster than it normally would be during Phase 1. If Phase 2 can’t handle the extra burden, a detoxification bottleneck results.
You can take steps to keep your liver detoxification system running smoothly. Diet has a strong effect on detoxification enzymes, and foods can help “regulate” or balance Phase 1 and 2 activity. Eating foods that support the liver can reduce your susceptibility to damage from toxins and to conditions such as multiple chemical sensitivity syndrome, chronic fatigue syndrome, and cancer. Research has shown that specific foods and nutrients not only have a beneficial effect on detoxification capability, but can also provide a safe and viable approach to treating a variety of immune disorders and toxicity syndromes.
Essential fatty acids are vital for Phase 1 detoxification, and the standard American diet does not provide an adequate supply of these vital nutrients. Essential fatty acid intake in the form of cold-water fish and flaxseed oils have a demonstrated ability to heighten detoxification. Other sources of essential fatty acids include edible oils, such as those made from sunflower seeds, walnuts, and sesame seeds; wheat germ; and supplements of black current seed, borage, or evening primrose oil.
Eating fresh fruits and vegetables daily is a good way to continually replenish your body’s store of glutathione, necessary for one of Phase 2 pathways. High-quality protein nourishes both the amino acid and the sulfation pathways. Vegetable sources of sulfur for the sulfation pathways include radishes, turnips, onions, celery, horseradish, string beans, watercress, kale, and soybeans. Eggs, fish, and meat are also excellent sulfur sources.
Cabbage, brussels sprouts, broccoli, citrus fruits, and lemon peel oils support Phase 2 activity. Studies have shown dramatic results from consuming broccoli sprout extract, which inhibits the activity of Phase 1 enzymes and, simultaneously enhances the Phase 2 glutathione pathway. Broccoli sprout extracts are especially beneficial for people who have frequent or high-level exposure to pesticides, exhaust fumes, paint fumes, cigarette smoke, or alcohol. Anyone who is exposed to known carcinogens will benefit from broccoli sprout extract.
Foods to Support Liver Detoxification
• Cabbage family
• Cold-water fish
• Flaxseed oil
• Fruits (fresh)
• Garlic
• Nuts and seeds
• Onions
• Safflower oil
• Sesame seed oil
• Sunflower seed oil
• Vegetables (fresh)
• Walnut oil
• Wheat germ and wheat germ oil
Nutritional Supplements to Support Liver Detoxification
• Bioflavonoids
• Black currant seed oil
• Borage oil
• Carotenes
• Coenzyme Q10
• Copper
• Evening primrose oil
• Folic acid
• Iron
• Lecithin
• Magnesium
• Manganese
• N-acetyl-cysteine
• Niacin
• Riboflavin
• Selenium
• Silymarin (milk thistle)
• Trace minerals
• Vitamin A
• Vitamin B6 (pyridoxine)
• Vitamin B12
• Vitamin C (ascorbic acid)
• Vitamin D
• Vitamin E
• Vitamin K
• Zinc
Tests that measure Phase 1 and Phase 2 enzymes take much of the guesswork out of estimating the severity of liver detoxification dysfunction, and can to some extent indicate whether a person is at special risk for cancer, neurological disease, chemical and drug sensitivity, and immune problems. Source
Detoxification, Phase II, Acetylation
Conjugation of toxins with acetyl-CoA is the primary method by which the body eliminates sulfa drugs. This system appears to be especially sensitive to genetic variation, with those having a poor acetylation system being far more susceptible to sulfa drugs and other antibiotics. While not much is known about how to directly improve the activity of this system, it is known that acetylation is dependent on thiamine, pantothenic acid, and vitamin C.
Detoxification, Phase II, Amino Acid Conjugation
The body manufactures five different types of amino acids that form this detoxification pathway: glycine, taurine, glutamine, arginine, and ornithine. Of these, glycine is the most important for the neutralization of toxins. In some cases, the body cannot make enough glycine to keep up with its own detoxification needs. Though not considered an essential amino acid because the body can make it, glycine production depends on an adequate intake of dietary protein. Individuals who eat a protein-deficient diet have trouble detoxifying environmental pollutants.
Glycine supplies can be depleted by lifestyle stresses. Benzoates for example, found in soft drinks, bind with glycine and rob the body’s store of it. One study found that people who consumed a large number of soft drinks had problems breaking down toluene, a common industrial organic solvent. Aspirin also slows down this detoxification pathway because it competes for available glycine in the liver. When the diet is supplemented with glycine, as well as the other nonessential amino acids, there is a noticeable improvement in the detoxification capabilities of many people.
Detoxification, Phase II, Glucoronidation Pathway
Glucuronidation, the combining of glucuronic acid with toxins, in Phase II can be reversed by Beta glucuronidase enzymes produced by pathological bacteria and cause toxins to be reabsorbed increasing toxicity. Many of the commonly prescribed drugs are detoxified through this pathway. It also helps to detoxify aspirin, menthol, vanillin (synthetic vanilla), food additives such as benzoates, and some hormones. Calcium d-glucurate, a natural ingredient found in certain vegetables and fruits can inhibit beta glucuronidase activity resulting in increased elimination of toxins.
Detoxification, Phase II, Glutathione Conjugation
One of the most important systems in Phase 2 is the glutathione conjugation pathway, which utilizes glutathione for the detoxification of deadly industrial toxins such as PCBs, and the breakdown of carcinogens. Its activity accounts for up to 60 percent of the toxins excreted in the bile. Glutathione also circulates through the bloodstream combating free radicals. No other conjugating substance is as versatile as glutathione and the body’s supply of it, most of which is produced by the liver, is easily depleted. Exposure to high levels of toxins exhausts reserves of glutathione, possibly increasing susceptibility to cancer. Chronic disease, HIV, and cirrhosis use up reserves of glutathione. Excessive exercise, which increases oxidative stress and free radical production, and alcohol consumption, which blocks glutathione production, also deplete glutathione in the blood.
Detoxification Function, Phase II, Methylation Pathway
Methylation and glutathione are very tightly intertwined. There is a critical metabolic intersection-a fork in the road-where cells must decide to either make more glutathione, or support more methylation. The overall balance between these two options is crucial to health. Your body can take homocysteine and convert it back to cysteine. Homocysteine is a metabolite of the essential amino acid methionine, and elevated levels have been associated with vascular disease. Homocysteine is created when methionine donates its methyl group to another molecule in a process known as methylation.
Methylation is a fundamental process of life which is intimately linked to redox status. In chemistry, a methyl group is a hydrocarbon molecule, or CH3. When a substance is methylated, it means that a CH3 molecule has been added to it. Methylation can regulate gene expression, protein function, even RNA metabolism. It can suppress viruses, even latent viruses or cancer viruses we are born with and can help us handle heavy metals. In the liver in particular, methylating a toxin helps change it to a form of the compound that can be more easily processed and excreted.
Methylation is an extremely broad and fundamental action that nature uses to regulate all kinds of processes. It regulates epigenetic changes-changes to gene expression that occur because of environmental factors-by affecting how DNA unravels during development. Some changes can be permanent for the whole lifespan and can even be passed down as many as three generations. That shows that the environment, through the process of methylation, can be quite a profound influence. There are 150-200 methyl transferase enzymes, and each enzyme can methylate multiple targets. So you can imagine methylation as a spider’s web within each cell, and that web branches out in many directions.
Methylation and glutathione are very tightly intertwined. There is a critical metabolic intersection-a fork in the road-where cells must decide to either make more glutathione, or support more methylation. The overall balance between these two options is crucial to health, and this occurs with homocysteine. When methionine gives away its methyl group, we’re left with homocysteine. And the body has to decide, should homocysteine be methylated, and go back into methionine, or should it be converted into cysteine, so that the body can make more of the antioxidant glutathione? This fundamental decision is made again and again by the body, and the overall balance is crucial to health. Too little glutathione and we will end up with free radical, oxidative damage. Not enough methylation, and many genes and viruses will not be properly regulated. Excess homocysteine, and the risk of vascular disease goes up.
Detoxification, Phase II, Sulfation Pathway
The weakest pathway in most people, from a dietary standpoint, is sulfation, the one responsible for the transformation of neurotransmitters, steroid hormones, drugs, industrial chemicals, phenolics (compounds derived from benzene, commonly used in plastics, disinfectants, and pharmaceuticals), and especially toxins from intestinal bacteria and the environment. Intake of too little dietary sulfur, a molecule that must come from our diets, is a cause of ineffective detoxification. If your exposure to substances that need to be detoxified via the sulfation pathway is high, but your sulfate reserves are low due to an inadequate diet, you will not be able to break down these toxins.
Studies have established a strong association between the function of the sulfation pathway and a variety of illnesses including Alzheimer’s disease, Parkinson’s disease, motor neuron disease, autism, primary biliary cirrhosis, rheumatoid arthritis, food sensitivity, and multiple chemical sensitivity. A comprehensive detoxification profile test identifies alterations in this pathway.
Energy Production Function
Understanding the liver’s role in energy production clarifies how a compromised liver can result in fatigue. The liver is intimately involved in supplying the body with energy. The liver converts glucose into glycogen, storing it for later use. When the body needs energy, liver glycogen can release glucose to provide fuel for creating a burst of energy. Additionally, if the body is low in carbohydrates, the liver can manufacture more from fat or proteins.
By producing, storing and supplying the body with glucose, the liver is a key player in preventing fatigue. A liver unaffected by disease releases glucose between meals, or whenever the cells need nourishment and energy. While a healthy liver maintains a steady level of energy throughout the day, one hampered by disease has a reduced ability to produce glucose, and less space to store it.
For those will liver disease, the continued, long-term response of the immune system contributes to fatigue. The release of neurotransmitters (chemicals in the brain) is part of a healthy immune system response. When the body is physically or emotionally stressed, the immune system activates, causing the brain to release the appropriate substance for self-protection. Liver disease causes a chronic, uncontrollable stress to the patient, weakening the immune system and decreasing the release of certain neurotransmitters.
Liver Fat Content
Fatty liver is a condition in which the cells of the liver accumulate abnormally increased amounts of fat. Although excessive consumption of alcohol is a very common cause of fatty liver (alcoholic fatty liver), there is another form of fatty liver, termed nonalcoholic fatty liver disease (nonalcoholic fatty liver disease), in which alcohol has been excluded as a cause. In nonalcoholic fatty liver disease, other recognized causes of fatty liver that are less common causes than alcohol also are excluded.
Nonalcoholic fatty liver disease is a manifestation of an abnormality of metabolism within the liver. The liver is an important organ in the metabolism (handling) of fat. The liver makes and exports fat to other parts of the body. It also removes fat from the blood that has been released by other tissues in the body, for example, by fat cells, or absorbed from the food we eat. In nonalcoholic fatty liver disease, the handling of fat by liver cells is disturbed. Increased amounts of fat are removed from the blood and/or are produced by liver cells, and not enough is disposed of or exported by the cells. As a result, fat accumulates in the liver.
Nonalcoholic fatty liver disease is classified as either fatty liver (sometimes referred to as isolated fatty liver or IFL) or steatohepatitis (NASH). In both isolated fatty liver and NASH there is an abnormal amount of fat in the liver cells, but, in addition, in NASH there is inflammation within the liver, and, as a result, the liver cells are damaged, they die, and are replaced by scar tissue.
Nonalcoholic fatty liver disease is important for several reasons. First, it is a common disease, and is increasing in prevalence. Second, NASH is an important cause of serious liver disease, leading to cirrhosis and the complications of cirrhosis–liver failure, gastrointestinal bleeding, and liver cancer. Third, nonalcoholic fatty liver disease is associated with other very common and serious non-liver diseases, perhaps the most important being cardiovascular disease that leads to heart disease and strokes. Fatty liver probably is not the cause of these other diseases, but is a manifestation of an underlying cause that the diseases share. Fatty liver, therefore, is a clue to the presence of these other serious diseases which need to be addressed. Source
Protein Metabolism The liver synthesizes non-essential amino acids from other amino acids, glucose and fatty acids. The enzymes alanine and aspartate transaminases convert amino acids that are in abundance to others that are needed by the body. A high concentration of these enzymes in the blood indicates liver damage. The liver makes most plasma proteins including albumin and produces coagulation factors. The liver breaks down proteins and removes the toxic ammonium ion by converting it to urea. Serum Globulin; a globulin or mixture of globulins occurring in blood serum and containing most of the antibodies of the blood. The serum globulin electrophoresis test measures the levels of proteins called globulins in the fluid part of a blood sample. This fluid is called serum, one of a group of proteins in blood serum with antibody qualities. The various types of serum globulins, designated alpha, beta, and gamma, have different specific properties. Serum total bile acid; Serum total bile acid (TBA) levels are used clinically as a sensitive and reliable index of hepatobiliary diseases. In the present study, to assess the clinical usefulness of determining TBA in interferon (IFN)-treated patients, changes in liver function test values, including TBA and liver histology, were examined in 36 chronic hepatitis C patients for 3 years after a sustained response to IFN treatment. Total bilirubin Bilirubin is a brownish yellow substance found in bile. It is produced when the liver breaks down old red blood cells. Bilirubin is then removed from the body through the stool (feces) and gives stool its normal color. A bilirubin test measures the amount of bilirubin in a blood sample. Total bilirubin and direct bilirubin levels are measured directly in the blood, whereas indirect bilirubin levels are derived from the total and direct bilirubin measurements. When bilirubin levels are high, the skin and whites of the eyes may appear yellow (jaundice). Jaundice may be caused by liver disease (hepatitis), blood disorders (hemolytic anemia), or blockage of the tubes (bile ducts) that allow bile to pass from the liver to the small intestine.

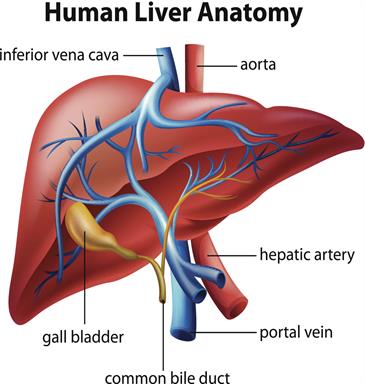
Lung Function
Airway Resistance RAW
The airway resistance, which in science and medicine is abbreviated as Raw. For air to move into or out of your lungs, it must want to, and it has to overcome friction, the force that stops two things from sliding past each other. Airway resistance is a measure of the resistance to lung airflow caused by friction. The resistance of your lung to airflow is a determinant of how easy it is to breathe; That’s why scientists like to measure it. Knowing the airway resistance helps doctors tell if your lungs are functioning normally.
The first formula for airway resistance involves figuring out the change in pressure from where air enters (your mouth) to where it ends up, the part of the lung called the alveoli. The pressure of the lung where air enters is the same as the pressure of the atmosphere, while the pressure of the alveoli (Palv) is determined by other factors. The most common unit of pressure used for the lung is centimeters of water (cmH2O). The other part involves flow rate (V dot), or how fast the air flows. Since air isn’t a solid, it’s most often measured by how much volume in liters it occupies, and since it moves so fast, time is usually measured in second.
Arterial Oxygen Content (PaCO2)
The definition is the amount of oxygen bound to hemoglobin (1.34 * Hb * SaO2) plus the oxygen dissolved in plasma (0.0031 * PaO2). The arterial oxygen content equation: CaO2 = (1.34 * Hb * SaO2) + (0.0031 * PaO2). The normal oxygen combining capacity is 1.39 mls/gram, however due to abnormal forms of hemoglobin such as carboxyhemoglobin and methemoglobin this value is reduced to 1.34 mls/gram. Hb is Hemoglobin, the normal Hb for males is 14-20 g/dl and females 12-15 g/dl. SaO2 is the percentage of available hemoglobin that is saturated with oxygen, this value is from a direct measurement of an arterial blood gas. 0.0031 is the solubility coefficient of oxygen at body temperature. PaO2 is the partial pressure of oxygen in arterial blood not bound to hemoglobin.
Total Lung Capacity (TLC)
The inspiratory capacity plus the functional residual capacity; the volume of air contained in the lungs at the end of a maximal inspiration. The average total lung capacity of an adult human male is about 6 litres of air. Tidal breathing is normal, resting breathing; the tidal volume is the volume of air that is inhaled or exhaled in only a single such breath.
Vital Capacity (VC)
This is the maximum amount of air a person can expel from the lungs after a maximum inhalation. It is equal to the sum of inspiratory reserve volume, tidal volume, and expiratory reserve volume.
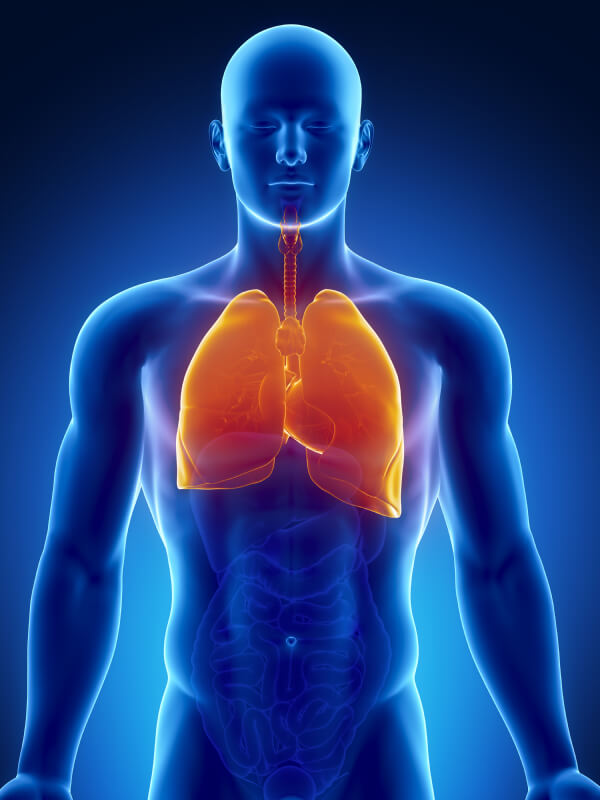
Body Reproductive Function: Female
Beta hCG Hormone
Cervicitis
This is inflammation of the cervix, which can be due to: Irritation, Infection, or Injury of cells that line the cervix. These irritated or infected tissues may become red, swollen, and ooze mucus and pus. They may also bleed easily when touched.
Cervicitis is common. It may be caused by a number of factors, including infections, chemical or physical irritations, and allergies. Determining the cause of cervicitis is important. If an infection is the problem, it can spread beyond the cervix to the uterus and fallopian tubes and into the pelvic and abdominal cavity and cause life-threatening infection. This may cause problems with fertility –the ability to become pregnant. Or it may cause problems with your unborn baby if you are already pregnant.
Endometriosis
This is a condition in which tissue that normally grows inside the uterus (endometrium) grows outside it. Most often this is on the ovaries, fallopian tubes, and tissue around the uterus and ovaries; however, in rare cases it may also occur in other parts of the body. The main symptoms are pelvic pain and infertility. Nearly half of those affected have chronic pelvic pain, while in 70% pain occurs during menstruation. Pain during sex is also common. Infertility occurs in up to half of women affected. Less common symptoms include urinary or bowel symptoms. About 25% of women have no symptoms. Endometriosis can have both social and psychological effects.
The cause is not entirely clear. Risk factors include having a family history of the condition. The areas of endometriosis bleed each month, resulting in inflammation and scarring. The growths due to endometriosis are not cancer. Diagnosis is usually based on symptoms in combination with medical imaging. Biopsy is the most sure method of diagnosis. Other causes of similar symptoms include pelvic inflammatory disease, irritable bowel syndrome, interstitial cystitis, and fibromyalgia.
Fallopian Tube Dysfunction
The fallopian tube may be blocked or damaged, preventing the egg from moving from the ovary to the uterus to be implanted. The fallopian tubes can sometimes be repaired, but in vitro fertilization is usually recommended.
Causes of fallopian tube problems include the following:
•Pelvic infections (such as pelvic inflammatory disease)
•A chlamydial infection
•Use of an intrauterine device if it causes a pelvic infection (which is rare)
•A ruptured appendix
•Surgery in the pelvis or lower abdomen
•A mislocated (ectopic) pregnancy in the fallopian tubes
Bacteria, such as those that can cause pelvic inflammatory disease or chlamydial infection (chlamydiae), can enter the vagina during sexual intercourse with a partner who has a sexually transmitted disease. The bacteria can spread from the vagina to infect the cervix. They may then spread upward, to the uterus and sometimes the fallopian tubes. Chlamydiae can infect the fallopian tubes without causing any symptoms. These infections may permanently damage the fallopian tubes, uterus, and surrounding tissue. Scar tissue may form and block the fallopian tubes.
Other causes of fallopian tube problems include abnormalities in the pelvis that block the tubes such as:
•Birth defects of the uterus and fallopian tubes
•Endometriosis
•Fibroids in the uterus
•Bands of scar tissue between adhesions in the uterus or pelvis
Fibroadenoma of Breast
Benign tumors characterized by an admixture of stromal and epithelial tissue. Since both fibroadenomas and breast cancer can appear as similar lumps, it is currently recommended to perform ultrasound analyses and possibly tissue sampling with subsequent histopathologic analysis in order to perform diagnosis. Unlike typical lumps from breast cancer, fibroadenomas are easy to move, with clearly defined edges.
There is research suggesting that fibrocystic breast disease correlates with iodine deficiency. From Dr. Brownstein’s book, Iodine Why You Need It and Why You Can’t Live Without It:
Animal studies have shown conclusively that an iodine deficient state can alter the structure and function of the breasts. After my own research and study, I concur with several investigators that iodine deficiency is a causative factor in breast cancer and fibrocystic breast disease. I believe it is essential that women have their iodine levels tested, and if it is shown there is an iodine deficiency, iodine supplementation should be initiated.
The breasts are one of the body’s main storage sites for iodine in the body. In an iodine-deficient state, the thyroid gland and the breasts will compete for what little iodine is available. Therefore, this will leave the thyroid gland and the breasts iodine depleted and can set the stage for illnesses such as goiter, hypothyroidism, autoimmune thyroid disease, breast illnesses including cancer, and cystic breast disease. In addition, other glandular tissues such as the ovaries which contain the second highest concentration of iodine in the body, will also be depleted in an iodine deficient state.
Hyperplasia of Mammary Glands
The most common type of proliferative breast condition is hyperplasia. There are two types of hyperplasia: usual hyperplasia (more common) and atypical hyperplasia (less common). In usual hyperplasia (the most common form of hyperplasia) the proliferating (dividing) cells look normal under a microscope. Women with usual hyperplasia have about twice the breast cancer risk of women without a proliferative breast condition. In atypical hyperplasia, the proliferating (dividing) cells look abnormal. Atypical hyperplasia is less common than usual hyperplasia. Women with atypical hyperplasia have about 3-5 times the breast cancer risk of women without a proliferative condition. One study found women diagnosed with atypical hyperplasia had about a 29 percent chance of developing breast cancer within 25 years. Atypical ductal hyperplasia (ADH) is not a form of breast cancer. Rather, it is a marker for women who may have a risk factor for developing breast cancer in the future. If you have a biopsy that shows atypical ductal hyperplasia in one of your breasts, your doctor will want to follow your breast health very carefully.
Mastitis
Mastitis is an infection and inflammation of the breast, usually the fatty tissue of the breast, that causes redness, pain and swelling. As this swelling pushes on the milk ducts, it causes pain.
Mastitis is usually caused by an infection with the bacteria Staphylococcus aureus. These bacteria are normally present on your skin, but cause problems when they enter the body. Bacteria causing mastitis enter through a break or crack in the skin of the breast, usually on the nipple. In fact, mastitis usually occurs in women who are breastfeeding because the nipples often become dry and irritated and can become cracked during nursing. This allows the bacteria to invade breast tissue, in particular the milk ducts and milk glands.
Mastitis in a nonbreastfeeding woman is more common after menopause than before. In very rare cases, this may indicate the presence of another primary disease, such as breast cancer. At the same time, a clogged milk duct can mimic mastitis. While a woman adjusts to breastfeeding a new infant, the milk ducts inside the breast can become clogged, causing tenderness, redness, lumps and even heat under the skin surface, but without infection. Source
Menopause
Menopause is the permanent end of menstruation. It is not a disease, but it can have a big impact on a woman’s well-being. Menopause can bring physical discomfort from hot flashes, night sweats, sleep issues, vaginal dryness and other symptoms. Age is the leading cause of menopause. It’s the end of a woman’s childbearing years, brought on by the ovaries gradually slowing down. Certain surgeries and medical treatment can induce menopause. Those include surgical removal of the ovaries (bilateral oophorectomy), chemotherapy, and pelvic radiation therapy. Having a hysterectomy (surgical removal of the uterus) without removing the ovaries does not lead to menopause, although you will not have periods anymore. There is no proven way to predict menopause age. It’s only after a woman has missed her periods for 12 straight months, without other obvious causes, that menopause can be confirmed.
Ovarian Cyst
There are various types of ovarian cysts, such as dermoid cysts and endometrioma cysts. However, functional cysts are the most common type. The two types of functional cysts include follicle and corpus luteum cysts.
During a woman’s menstrual cycle, an egg grows in a sac called a follicle. This sac is located inside the ovaries. In most cases, this follicle or sac breaks open and releases an egg. But if the follicle doesn’t break open, the fluid inside the follicle can form a cyst on the ovary. Follicle sacs typically dissolve after releasing an egg. But if the sac doesn’t dissolve and the opening of the follicle seals, additional fluid can develop inside the sac and this accumulation of fluid causes a corpus luteum cyst.
Other types of ovarian cysts include: dermoid cysts which are sac-like growths on the ovaries that can contain hair, fat, and other tissue, cystadenomas: non-cancerous growths that can develop on the outer surface of the ovaries, endometriomas: tissues that normally grow inside the uterus can develop outside the uterus and attach to the ovaries, resulting in a cyst.
Some women develop a condition called polycystic ovary syndrome. This condition means the ovaries contain a large number of small cysts. It can cause the ovaries to enlarge, and if left untreated, polycystic ovaries can cause infertility. (see iodine, under minerals)
Often times, ovarian cysts do not cause any symptoms. However, symptoms can appear as the cyst grows. Symptoms may include:
•abdominal bloating or swelling
•painful bowel movements
•pelvic pain before or during the menstrual cycle
•painful intercourse
•pain in the lower back or thighs
•breast tenderness
•nausea and vomiting
Severe symptoms of an ovarian cyst that require immediate medical attention include:
•severe or sharp pelvic pain
•fever
•faintness or dizziness
•rapid breathing
These symptoms can indicate a ruptured cyst or an ovarian torsion. Both complications can have serious consequences if not treated early.
Ovulation
It was commonly believed that we always ovulated whenever we were having regular menstrual flow with normal-length menstrual cycles of 21-35 days apart. CeMCOR and other groups of scientists have now shown that variability in ovulation and huge variation in the amount of progesterone that each menstrual cycle makes are very common. This frequent but not obvious cycle variation is called an “ovulatory disturbance” that includes not releasing an egg (anovulation) as well as releasing an egg with too short a time from egg-release to the next flow (short luteal phase). Ovulatory disturbances are silent within regular and normal menstrual cycles. It is still true, however, that irregular or far apart cycles are even more likely to have ovulatory disturbances. Who’s at increased risk for silent, ovulatory disturbances? We don’t know for sure because few studies have tracked women’s cycles for ovulation over extended periods. Adolescent and young women (in the first 10 years after first period or menarche) are more likely to have ovulatory disturbances; irregular flow is also common in the first year.
Also, women in perimenopause have increasing ovulatory disturbances; luteal lengths can be normal but progesterone production too low during this life phase. Obesity is associated with ovulatory disturbances, as is cigarette smoking. But probably the most common reason for having a regular cycle with too little or no progesterone production is being under stress: the “threat” can be physical (illness, over-exercise), emotional (break-up with a partner, grief, depression), nutritional (not being able to afford or get to, enough nutritious food or not eating enough for body needs), social (bullying, sexual abuse, social isolation) or spiritual (not feeling life has fundamental meaning). Thus CeMCOR investigators have come to see a normally ovulatory, regular menstrual cycle as a sign of health and well-being. Source
Pelvic Inflammatory Disease (PID)
This is an infection of the organs of a women’s reproductive system. They include the uterus, ovaries, fallopian tubes, and cervix. It’s usually caused by a sexually transmitted infection (STI), like chlamydia or gonorrhea, and is treated with antibiotics.
You might not notice any symptoms of PID early on. But as the infection gets worse, you can have:
•Pain in your lower belly and pelvis
•Heavy discharge from your vagina with an unpleasant odor
•Bleeding between periods
•Pain during sex
•Fever and chills
•Pain when you pee or a hard time going
Call your doctor right away if you have any of these.
PID can cause serious problems if it’s not treated. For example, you might have trouble getting pregnant or have pain in your pelvic area that doesn’t go away. Source
Premenstrual Syndrome (PMS)
Premenstrual syndrome (PMS) is a combination of emotional, physical, psychological, and mood disturbances that occur after a woman’s ovulation, typically ending with the onset of her menstrual flow. The most common mood-related symptoms are irritability, depression, crying, oversensitivity, and mood swings. The most common physical symptoms are fatigue, bloating, breast tenderness (mastalgia), acne, and appetite changes with food cravings.
A more severe form of PMS, known as premenstrual dysphoric disorder (PMDD), also known as late luteal phase dysphoric disorder, occurs in a smaller number of women and leads to significant loss of function because of unusually severe symptoms. The American Psychiatric Association characterizes PMDD as a severe form of PMS in which anger, irritability, and anxiety or tension are especially prominent.
About 90% of women experience premenstrual symptoms at some point in their lifetime. The true incidence of PMS has often been overestimated by including all women who experience any physical or emotional symptoms prior to menstruation. It is estimated that clinically significant PMS (which is moderate to severe in intensity and affects a woman’s functioning) occurs in 20% to 30% of women. It is generally most severe in women in their 4th decade of life.
Vaginitis
Vaginitis is inflammation of the vagina. In premenopausal women, infection is the most common cause. After menopause, a low level of estrogen often leads to vaginal atrophy (atrophic vaginitis). Vaginitis also can be the result of an allergic reaction to an irritating chemical, such as a spermicide, douche or bath soap.
Almost all infectious vaginitis is caused by one of three infections:
Bacterial vaginosis is a change in the type of bacteria that normally live in the vagina, and it is the most common cause of an abnormal vaginal discharge or an unpleasant vaginal odor. In bacterial vaginosis, normal Lactobacillus bacteria are replaced by other bacteria, including Prevotella, Mobiluncus, G. vaginalis, and Mycoplasma hominis. The exact reason for this change is unknown. In pregnant women, bacterial vaginosis can increase the risk of premature delivery.
Candida vaginal infections, also called vaginal yeast infections, typically are caused by the Candida albicans fungus. During a lifetime, 75% of all women are likely to have at least 1 Candida vaginal infection, and up to 45% have 2 or more. Women tend to be more susceptible to vaginal yeast infections if their bodies are under stress from poor diet, lack of sleep or illness, or if they are pregnant, taking antibiotics or birth control pills or douching too often. Women with diabetes or human immunodeficiency virus (HIV) are more likely to have recurrent yeast infections.
Trichomonas vaginitis, also called trichomoniasis, is a sexually transmitted disease (STD) caused by a microscopic one-celled organism called Trichomonas vaginalis. Trichomonas causes inflammation of the vagina, cervix and urethra in women. In pregnant women, Trichomonas infections also can increase the risk of premature rupture of the membranes and preterm delivery.
Symptoms:
Bacterial vaginosis – Bacterial vaginosis causes an abnormal grayish-white vaginal discharge with a foul-smelling vaginal odor.
Candida vaginitis – Candida vaginitis can cause the following symptoms:
Vaginal itch or soreness
A thick cheese-like vaginal discharge
Burning discomfort around the vaginal opening, especially if urine touches the area
Pain or discomfort during sexual intercourse
Trichomonas – In women, Trichomonas organisms can live in the vagina for many years without causing any symptoms. If symptoms occur, they can include:
A yellow-green, foul-smelling vaginal discharge
Vaginal pain or itching
Irritation and inflammation around the vaginal opening
Discomfort in the lower abdomen
Vaginal pain during sexual intercourse
Burning discomfort during urination
Symptoms can be worse during a menstrual period.
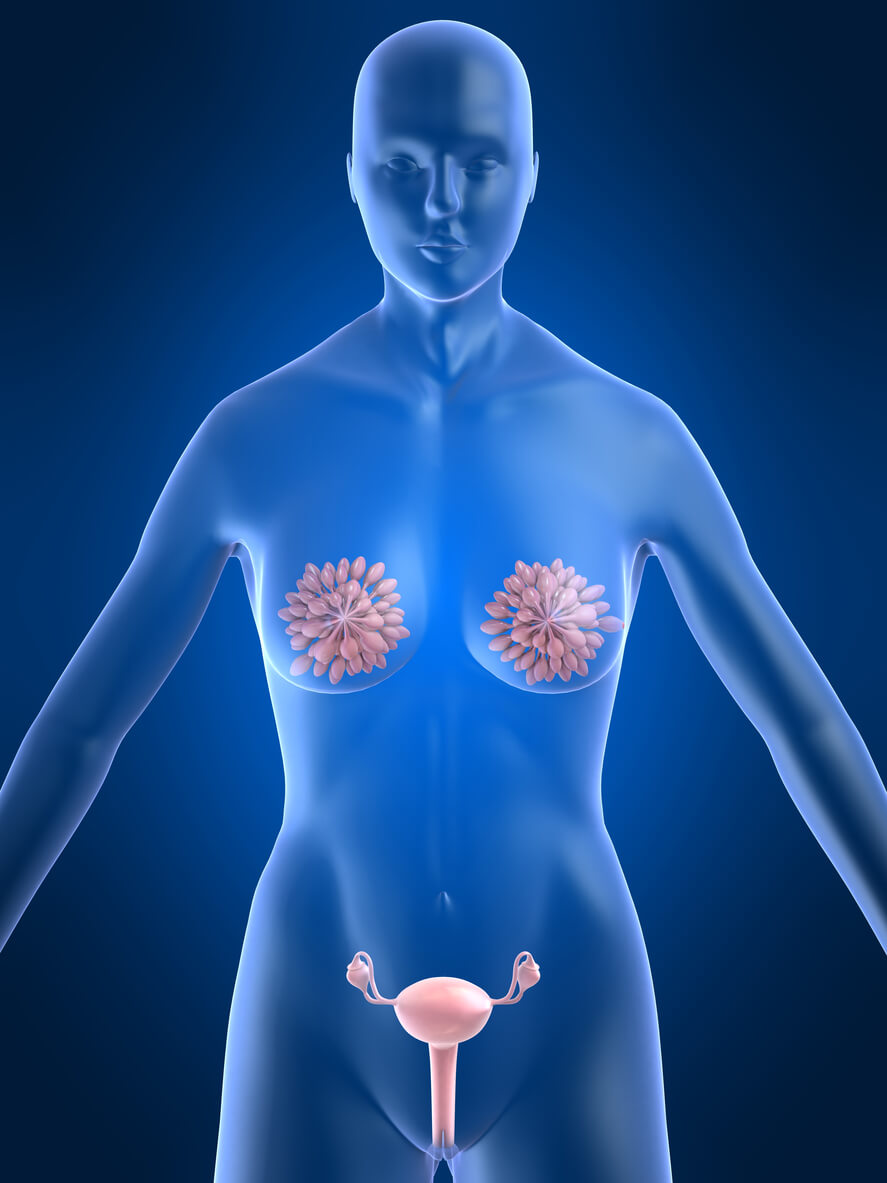
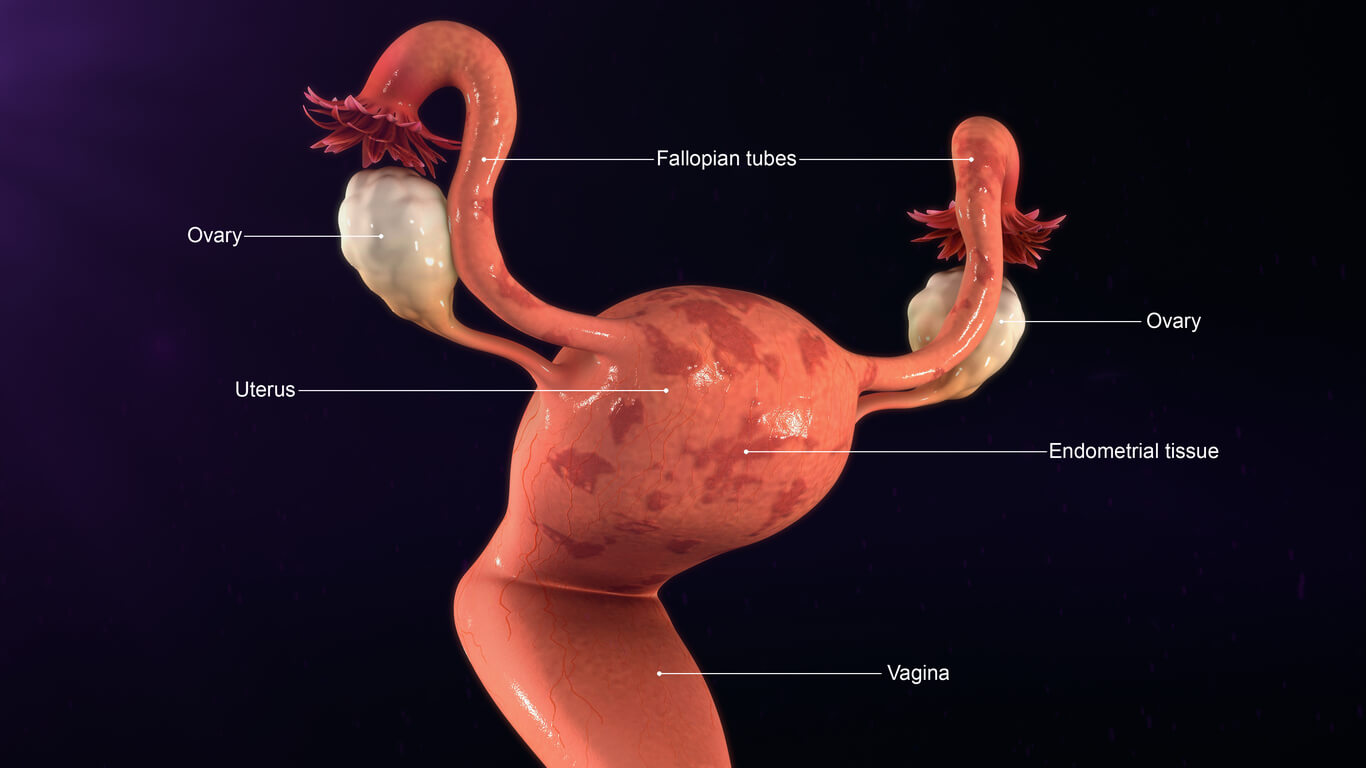
Body Reproductive Function: male
Erection Transmitter
As an autonomic nervous system response, an erection may result from a variety of stimuli, including sexual stimulation and sexual arousal, and is therefore not entirely under conscious control. Erections during sleep or upon waking up are known as nocturnal penile tumescence (NPT). Absence of nocturnal erection is commonly used to distinguish between physical and psychological causes of erectile dysfunction and impotence.
Liquefaction Time
Prostatic Calcification
Prostate calcification is another name for the calcified stones that can develop in the prostate. Although prostate calcification can be nothing to worry about, it can also be a sign of a more serious underlying condition. One of the most common causes of such stones is BPH, benign prostatic hypertrophy.
Prostatic Hyperplasia
Benign prostatic hyperplasia (BPH), also called benign enlargement of the prostate (BEP or BPE), is a noncancerous increase in size of the prostate. BPH involves hyperplasia of prostatic stromal and epithelialcells, resulting in the formation of large, fairly discrete nodules in the transition zone of the prostate. BPH involves hyperplasia (an increase in the number of cells) rather than hypertrophy (a growth in the size of individual cells), but the two terms are often used interchangeably, even among urologists.
Prostatitis Syndrome
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is characterized by pelvic or perineal pain without evidence of urinary tract infection, lasting longer than 3 months, as the key symptom. Symptoms may wax and wane. Pain can range from mild to debilitating. Pain may radiate to the back and rectum, making sitting uncomfortable. Pain can be present in the perineum, testicles, tip of penis, pubic or bladder area. Dysuria, arthralgia,myalgia, unexplained fatigue, abdominal pain, constant burning pain in the penis, and frequency may all be present. Frequent urination and increased urgency may suggest interstitial cystitis (inflammation centered in bladder rather than prostate). Post-ejaculatory pain, mediated by nerves and muscles, is a hallmark of the condition, and serves to distinguish CP/CPPS patients from men with BPH or normal men. Some patients report low libido, sexual dysfunctionand erectile difficulties.
PSA
PSA is a protein produced by the prostate gland. Although most PSA is carried out of the body in semen, a very small amount escapes into the blood stream.
The PSA value used most frequently as the highest normal level is 4 ng/mL (nanograms per milliliter). However, since the prostate gland generally increases in size and produces more PSA with increasing age, it is normal to have lower levels in young men and higher levels in older men. Age-specific PSA levels are as follows (age group, upper normal): (40 – 49, 2.5), (50 – 59, 3.5), (60 – 69, 4.5), (70 – 79, 6.5). The use of age-specific PSA ranges for the detection of prostate cancer is controversial. Not all studies have agreed that this is better than simply using a level of 4 ng/mL as the highest normal value.
Semen Volume
This is a measure of how much semen is present in one ejaculation.
Sperm Count
This counts the number of sperm present per milliliter (mL) of semen in one ejaculation.
Sperm Fructose Level
This is a measure of the amount of a sugar called fructose in the semen. The fructose provides energy for the sperm.
Sperm Morphology
This is a measure of the percentage of sperm that have a normal shape.
Sperm Motility Rate
This is a measure of the percentage of sperm that can move forward normally. The number of sperm that show normal forward movement in a certain amount of semen can also be measured. This is called motile density.
Sperm pH
This is a measure of the acidity (low pH) or alkalinity (high pH) of the semen.
Sperm White Blood Cell Count
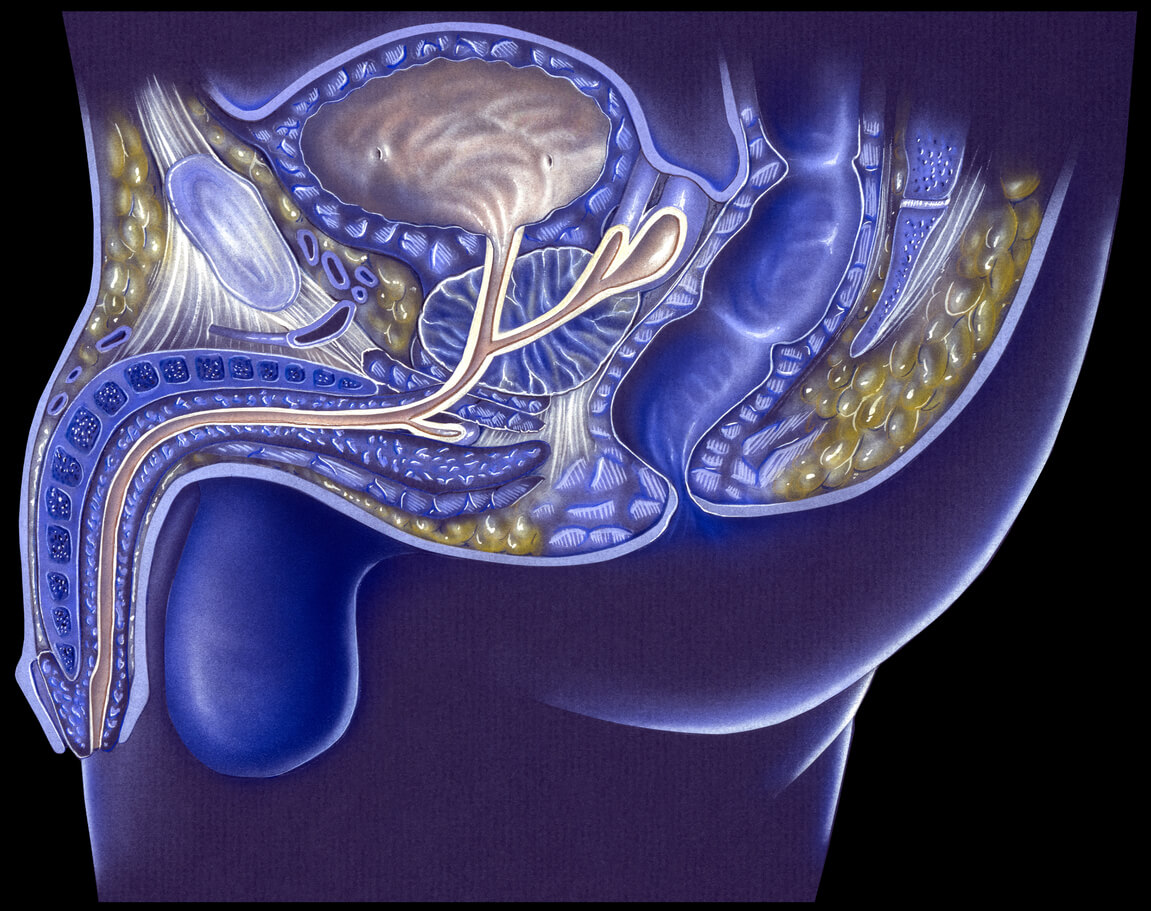

Skin Index
Skin Callous
A callus (or callosity) is a toughened area of skin which has become relatively thick and hard in response to repeated friction, pressure, or other irritation. Rubbing that is too frequent or forceful will cause blisters rather than allow calluses to form. Since repeated contact is required, calluses are most often found on feet because of frequent walking. Calluses are generally not harmful, but may sometimes lead to other problems, such as skin ulceration or infection.
Skin Collagen
Collagen is a vital fibrous protein that is found all throughout the body; it connects and supports tissues including skin, bone, muscles, tendons, cartilage and organs. It’s the main protein in connective tissue and is responsible for skin firmness and suppleness. s your skin loses collagen, it loses elasticity and, on average, we lose about 1% of our collagen every year after the age of 20!
The more collagen we lose, the more fine lines and wrinkles appear, which is why it is essential that we work to increase our collagen levels as we age. We accomplish this not only through topical products, but also by living a healthy lifestyle, which addresses nutritional and emotional needs for optimal skin health. Try eating foods that are rich in collagen boosting ingredients such as embryonic foods that contain amino acids (eggs, beans and seeds), antioxidants, which inhibit damage to collagen (pomegranates and goji berries are great) and good fats (like walnuts and avocado). Also, do your best to avoid exposure to sun, pollution, cigarettes, alcohol, drugs, pesticides, toxins and stress, which all contribute to collagen loss and ultimately older looking skin.
Skin Elasticity
The protein elastin is found in connective tissues throughout the body. It is notably found in the extracellular matrix of the skin as well as the internal organs of the body. The elastin protein is flexible and gives many tissues their elasticity. The ability of skin to stretch and then return to its normal state afterward is called elasticity. Unfortunately, a loss of elasticity in the skin is a natural part of aging known as elastosis. Elastosis may be worse in people who spend a lot of time in the sun. UVA (aging) and UVB (burning) rays weaken the skin’s support system of collagen and elastin – thereby accelerating the skin’s aging process.
Skin Free Radical
Free radicals are charged chemical particles of oxygen that enter into destructive chemical bonds with organic substances such as proteins. The result is an oxidation, or chemical burning, of the substance, which destroys it. Protein is denatured, genes may be broken and dangerous residual substances may result from the chemical changes. Exposure to sunlight is known to lead to oxidative destruction of the skin, including increased incidence of skin cancer and the collagen-destroying processes causing wrinkling. Strenuous aerobic activity has been associated with increased free radical formation. The evidence of free radical production leading to oxidation and tissue damage is real. Free radicals cause damage to our skin’s DNA that can speed along skin aging. This is called the free radical theory of aging.
Sleep enables the body to reverse everyday free radical damage by replenishing energy, building new cells and repairing connective tissue. Because sleep is an ideal time for cellular renewal and overall repair for the skin and other organs, poor sleep is quite apparent in the complexion.
Other things that can support the body in fighting free radicals include Vitamin C, Vitamin E, and melatonin. The combination of vitamin C, vitamin E and melatonin may represent one of the most effective ways to get enough of these antioxidants into the skin to impede collagen destruction, encourage collagen production, reduce facial wrinkles and undo sun damage.
Foods such as citrus fruits, carrots and pomegranates are high on the long list of healthy sources of antioxidants. Green tea is a great source of the powerful antioxidant group called catechins. Lycopene is perhaps the most potent dietary antioxidant. It is found in abundant supply in tomatoes, carrots and other yellow, red and orange fruits and vegetables. Cold water fish provides essential omega-3’s which can also be beneficial.
Skin Grease
Oil(sebum) is produced by sebaceous glands and secreted through pores. Sebaceous glands are microscopic exocrine glands in the skin that secrete an oily matter called sebum, to lubricate and waterproof the skin and hair. In humans, they are in the face and scalp, everywhere, except the palms of the hands and soles of the feet. The type of secretion of the sebaceous glands is referred to as holocrine.Nasal sebum, also known as nose grease/oil, is grease removed from the surface of the human nose. The pores of the lateral creases (where the nose joins the face) of the exterior of the nose create and store more oil and grease than pores elsewhere on the human body, forming a readily available source of small quantities of grease or oil. The grease is a particularly oily form of sebum.
Skin Immunity
Skin immunity is a property of skin that allows it to resist infections from pathogens. In addition to providing a passive physical barrier against infection, the skin also contains elements of the innate and adaptive immune systems which allows it to actively fight infections.
Skin Inflammation
Skin inflammation can be characterized as acute or chronic. Acute inflammation can result from exposure to UV radiation (UVR), ionizing radiation, allergens, or to contact with chemical irritants (soaps, hair dyes, etc.). This type of inflammation is typically resolved within 1 to 2 weeks with little accompanying tissue destruction. In contrast, chronic inflammation results from a sustained immune cell mediated inflammatory response within the skin itself. This inflammation is long lasting and can cause significant and serious tissue destruction. When the skin is exposed to a “triggering” stimulus, such as UV radiation, an irritant (e.g. soaps or fragrances), or to allergens, the cells in the skin produce a variety of inflammatory “hormones” called cytokines and chemokines. These “inflammatory messengers” bind to specific receptors on target cells and stimulate the production of additional inflammatory signaling “hormones”. Some of these cause vasodilation while others activate nerve cells. Still other cytokines cause immune cells to leave the blood and migrate into the skin where they then produce more inflammatory hormones, as well as enzymes, free radicals, and chemicals that damage the skin. The result of the initial triggering event is the amplification of a large inflammatory response that, while designed to help the skin fight infection from invading bacteria, actually causes considerable damage to the skin.
Skin Melanin
This the pigment that gives human skin, hair, and eyes their color. Dark-skinned people have more melanin in their skin than light-skinned people have. Melanin is produced by cells called melanocytes. It provides some protection again skin damage from the sun, and the melanocytes increase their production of melanin in response to sun exposure. Freckles, which occur in people of all races, are small, concentrated areas of increased melanin production.
Skin Moisture
Skin has what is called a “moisture barrier.” This is the barrier of the skin that is responsible for keeping moisture in and bad bacteria out (keeping in mind that there’s always a mix of yeast and p. acnes bacteria, among others, present on the skin). However, this barrier can become stripped away, which makes skin lose moisture at a rapid rate, leading to the production of more sebum (oil) to “compensate,” as well as more bacteria to feed on the dead skin cells and sebum. As a result, skin becomes more sensitive, dry, oily, dull, and potentially broken out. It also will heal slower and respond more viciously to skin remodelers (actives such as AHA, BHA, BP, sulfur, and tretinoin).
Dehydrated skin can present itself differently in many people. it usually has two or more of the following symptoms:
Lackluster, dull
Sallow or “tired,” almost sickly looking
Has no real “bounce” or spring to it — looks dry and wrinkly when pulled taut
Prone to congestion, particularly closed comedones
Burns and feels irritated when applying bland moisturizers
Feels very dry and tight when cleansed
Very oily in appearance, but feels bone dry in places and flakes very badly in spots
However, before explaining methods to fix dehydrated skin, you need to first understand why skin becomes dehydrated.
Information from these sites:
https://www.nuskin.com/en_US/corporate/company/science/personal_care_science/collagen.html
https://www.makeup.com/what-are-free-radicals
http://www.medicinenet.com/script/main/art.asp?articlekey=4340
http://burkewilliamsspa.com/2014/10/23/5-reasons-must-moisturize-skin-2/
http://www.dermamedics.com/inflammation_id55.html
https://www.murad.com/blog/collagen-elastin-the-skins-youth-proteins/
http://www.skininc.com/skinscience/ingredients/Antioxidants-Free-Radicals-and-Skin-Care-227888041.html#sthash.vSxid650.dpuf

Thyroid Function
Thyroid Function (TFTs)
If you have an autoimmune condition, it can disrupt your production of thyroglobulin. An autoimmune condition happens when your immune system creates antibodies that attack your body’s own healthy cells. When your immune system attacks the thyroid, it often targets thyroglobulin. This causes it to produce antithyroglobulin antibodies.
Your thyroid is a gland located in your neck. It releases hormones that control your metabolism. It produces a number of different proteins, including thyroglobulin. Your thyroid uses thyroglobulin to make the active thyroid hormones.
If you have an autoimmune condition, it can disrupt your production of thyroglobulin. An autoimmune condition happens when your immune system creates antibodies that attack your body’s own healthy cells. When your immune system attacks the thyroid, it often targets thyroglobulin. This causes it to produce antithyroglobulin antibodies.
If you do have small amounts in your blood, it may be a sign of certain health problems, such as:
•Type 1 diabetes
•Pernicious anemia, a drop in red blood cells caused by a vitamin B-12 deficiency
•Collagen vascular diseases, such as rheumatoid arthritis and scleroderma
•Thyroid cancer
If you have high levels of antithyroglobulin antibodies in your blood, it may be a sign of serious autoimmune disorder, such as Graves’ disease or Hashimoto thyroiditis.
In some cases, you may have antithyroglobulin antibodies in your blood without any specific complications. If you test positive for these antibodies, and your doctor can’t identify an underlying cause, they may monitor you for emerging health problems.
Anti-Thyroid Peroxidase Antibody
An anti-thyroid microsomal antibody test is also called a thyroid peroxidase test. It measures anti-thyroid microsomal antibodies in your blood. Your body produces these antibodies when cells in your thyroid become damaged. If you have an autoimmune disease or thyroid disorder, your antibody levels may rise. A positive test indicates an abnormal result and may be due to a variety of conditions, including:
Hashimoto’s thyroiditis, which is a swelling of the thyroid gland that often results in reduced thyroid function
Graves’ disease, which is an autoimmune disorder in which the thyroid gland is overactive
Granulomatous thyroiditis, or subacute thyroiditis, which is a swelling of the thyroid gland that usually follows an upper respiratory infection
Autoimmune hemolytic anemia, which is a drop in the number of red blood cells due to increased destruction by the immune system
nontoxic nodular goiter, which is an enlargement of the thyroid gland with cysts called nodules
Sjogren’s syndrome, which is an autoimmune disorder in which the glands that produce tears and saliva are damaged
Systemic lupus erythematosus, which is a long-term autoimmune disorder affecting your skin, joints, kidneys, brain, and other organs
Rheumatoid arthritis
Thyroid cancer
Women with high levels of anti-thyroid microsomal antibodies have a higher risk of:
Miscarriage
Preeclampsia
Premature birth
Difficulty with in vitro fertilization
Having anti-thyroid antibodies in your blood doesn’t automatically mean you have a thyroid disease. However, you may be at increased risk for future thyroid disease, and your doctor may want to monitor your condition. For unknown reasons, the risk tends to be higher in women.
Calcitonin
The calcitonin test is primarily used to help diagnose C-cell hyperplasia and medullary thyroid cancer, to evaluate the effectiveness of treatment, and to monitor those affected for recurrence. It is also ordered to screen for medullary thyroid cancer in family members of people with multiple endocrine neoplasia type 2 (MEN 2). C-cell hyperplasia and medullary thyroid cancer are two rare conditions in which excessive amounts of calcitonin are produced. C-cell hyperplasia is a benign condition that may or may not progress to become medullary thyroid cancer.
A low level of calcitonin means that it is unlikely that symptoms are due to C-cell hyperplasia or medullary thyroid cancer. An elevated concentration of calcitonin means that excessive amounts are being produced. Significantly elevated levels of calcitonin are a good indicator of C-cell hyperplasia or medullary thyroid cancer; however, the healthcare practitioner will use other procedures, such as a thyroid , scan, biopsy and ultrasound, to establish the diagnosis.
With successful treatment for medullary thyroid cancer, which may involve removal of the thyroid gland and often some surrounding tissues, calcitonin levels will usually fall to very low levels. If the values stay low over time, then it is likely that the treatment was effective. In some cases, calcitonin levels will fall but remain moderately elevated after treatment. This means that some calcitonin-producing tissue remains. Healthcare practitioners will monitor calcitonin and watch for increases over time. If calcitonin levels begin to rise, then it is likely that there is a recurrence of medullary thyroid cancer.
With medullary thyroid cancer and C-cell hyperplasia, other thyroid tests, such as T4, T3, and TSH, are usually normal while calcitonin levels are elevated.
Calcitonin levels may also be elevated with lung, breast, and pancreatic cancers, insulinomas (tumor in the pancreas that produces too much insulin), and rare pancreatic tumors called VIPomas (cancer that usually grows from islet cells in the pancreas).
Concentrations of calcitonin may be increased with use of drugs such as epinephrine, glucagon, and oral contraceptives, and are normally higher in newborns as well as in women during pregnancy.
Other conditions with elevated calcitonin include: Intestinal, gastric, or bronchial carcinoid tumors, chronic renal failure, Zollinger-Ellison syndrome, and pernicious anemia.
rT3, Reverse T3
This is a competitive inhibitor to T3 and T4. Leptin resistance is directly correlated with reverse T3. Leptin is a hormone that controls all of energy metabolism in the body. It controls all the other hormones in the body as well. If it is not working well, the rest of your hormones are going to show clinical problems as well. Many people think they have thyroid issues when they actually have leptin resistant. One becomes leptin resistant when the brain no longer recognizes the leptin signal sent from our fat cells. Testing leptin is easy to do but rarely done in medicine today. Biochemically it can be done with thereverse T3 test. Leptin resistance completely turns off your thyroid gland making it so you cannot burn fat in your muscles because it down regulates your basal metabolic rate.
T3, Free (Free Triiodothyronine)
Measures the free, unbound levels of the hormone triiodothyronine – the active thyroid hormone at the cellular level. Because the free levels of T3 represent immediately available hormone, free T3 is thought to better reflect the patient’s hormonal status than total T3.
Elevated Free T3 – Elevated Free T3 may be indicative of hyperthyroidism.
Low Free T3 – Low Free T3 levels below the reference range may be indicative of hypothyroidism.
Optimal Free T3 – Some integrative physicians and hormone experts state that if free T3 is not in the top half – or even the top quarter – of the reference range, it is not optimal.
T4, Free
This measures the free, unbound thyroxine levels (the storage hormone), in your bloodstream. Free T4 is typically elevated in hyperthyroidism, and lowered in hypothyroidism. Free or unbound T4 levels represent the level of hormone available for uptake and use by cells. Because the free levels of T4 represent immediately available hormone, free T4 is thought to better reflect the patient’s hormonal status than total T4.
TSH, Thyroid-Stimulating Hormone
This is a hormone that stimulates the thyroid gland to produce T3 and T4. Releasing hormone from the hypothalamus causes the release of the hormone TSH from the anterior pituitary gland, which finally allows the release of the hormones T3 and T4 from the thyroid gland.
You could have a perfectly functioning thyroid; but if your pituitary gland is not sending over the correct TSH levels to your thyroid telling it to go to work… Then it doesn’t. If that is the case, you have a lack of T4 & T3 hormones being produced in your body; a condition known as “hypothyroidism”.
If your pituitary gland is constantly bombarding your thyroid with high TSH levels, it kicks the thyroid into overdrive, and your thyroid starts producing too much T3 & T4 hormones. This is what causes the condition known as “hyperthyroidism”.
When the thyroid does not produce enough thyroid hormones, the pituitary detects this reduction in thyroid hormones, and it tries to stimulate the thyroid into action by producing and sending over more TSH. This is the pituitary gland’s effort to return the TSH levels to “normal” and balance the thyroid’s function. Therefore, higher TSH levels than normal suggests a thyroid that is under-active and not doing its job of producing thyroid hormone. So, in general, higher levels of thyroid stimulating hormone equals an under-active thyroid; or hypothyroidism.
And the opposite is true. If the thyroid is overactive and producing too much thyroid hormone, the pituitary senses that there is a thyroid hormone overload circulating through the system.
The pituitary then usually slows or shuts down thyroid stimulation, so that the thyroid will slow down its production of the T3 & T4 hormones. This drop in TSH is the pituitary gland’s attempt to return circulating T3 & T4 hormone levels to normal. Therefore, the TSH test results will show lower than normal TSH when the thyroid is overactive. So, in general, lower TSH levels equals an overactive thyroid; or hyperthyroidism.
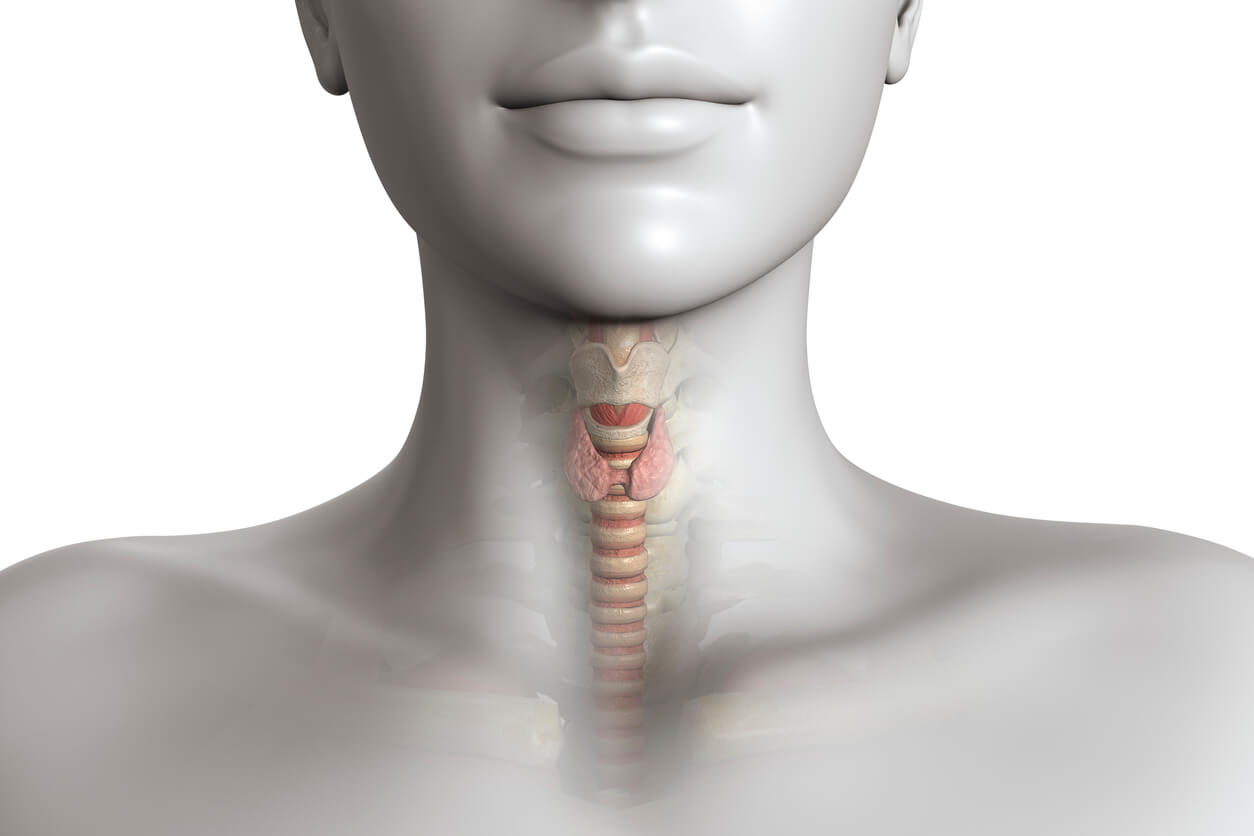
The thyroid is a butterfly-shaped gland that sits low on the front of the neck. Your thyroid sits just below your Adam’s apple, along the front of the windpipe. The thyroid has two side lobes, connected by a bridge in the middle. When the thyroid is its normal size, you will not even be able to feel it. The thyroid is responsible for controlling energy consumption by releasing hormones that control your metabolism. It also regulates body temperature, weight, and heart rate.
Here’s a perfect example of what your thyroid does; it works very similar to the thermostat in your house. If the thyroid is too active and produces too much of the T4 and T3 hormones (which control your body’s metabolism), it’s like having a thermostat that’s set too high…So the house gets overheated. If it’s not active enough, it’s set too low and the house is too cold. And if it’s making just the right amount of T4 and T3 hormones, then it keeps the temperature just right.
Anti-Thyroglobulin Antibody; Your thyroid uses thyroglobulin to make the active thyroid hormones.
If you have an autoimmune condition, it can disrupt your production of thyroglobulin. An autoimmune condition happens when your immune system creates antibodies that attack your body’s own healthy cells. When your immune system attacks the thyroid, it often targets thyroglobulin. This causes it to produce antithyroglobulin antibodies.
Your thyroid is a gland located in your neck. It releases hormones that control your metabolism. It produces a number of different proteins, including thyroglobulin. Your thyroid uses thyroglobulin to make the active thyroid hormones.
If you have an autoimmune condition, it can disrupt your production of thyroglobulin. An autoimmune condition happens when your immune system creates antibodies that attack your body’s own healthy cells. When your immune system attacks the thyroid, it often targets thyroglobulin. This causes it to produce antithyroglobulin antibodies.
If you do have small amounts in your blood, it may be a sign of certain health problems, such as:
•Type 1 diabetes
•Pernicious anemia, a drop in red blood cells caused by a vitamin B-12 deficiency
•Collagen vascular diseases, such as rheumatoid arthritis and scleroderma
•Thyroid cancer
If you have high levels of antithyroglobulin antibodies in your blood, it may be a sign of serious autoimmune disorder, such as Graves’ disease or Hashimoto thyroiditis.
In some cases, you may have antithyroglobulin antibodies in your blood without any specific complications. If you test positive for these antibodies, and your doctor can’t identify an underlying cause, they may monitor you for emerging health problems.
Anti-Thyroid Peroxidase Antibody; An anti-thyroid microsomal antibody test is also called a thyroid peroxidase test. It measures anti-thyroid microsomal antibodies in your blood. Your body produces these antibodies when cells in your thyroid become damaged. If you have an autoimmune disease or thyroid disorder, your antibody levels may rise. A positive test indicates an abnormal result and may be due to a variety of conditions, including:
Hashimoto’s thyroiditis, which is a swelling of the thyroid gland that often results in reduced thyroid function
Graves’ disease, which is an autoimmune disorder in which the thyroid gland is overactive
Granulomatous thyroiditis, or subacute thyroiditis, which is a swelling of the thyroid gland that usually follows an upper respiratory infection
Autoimmune hemolytic anemia, which is a drop in the number of red blood cells due to increased destruction by the immune system
nontoxic nodular goiter, which is an enlargement of the thyroid gland with cysts called nodules
Sjogren’s syndrome, which is an autoimmune disorder in which the glands that produce tears and saliva are damaged
Systemic lupus erythematosus, which is a long-term autoimmune disorder affecting your skin, joints, kidneys, brain, and other organs
Rheumatoid arthritis
Thyroid cancer
Women with high levels of anti-thyroid microsomal antibodies have a higher risk of:
miscarriage
preeclampsia
premature birth
difficulty with in vitro fertilization
Having anti-thyroid antibodies in your blood doesn’t automatically mean you have a thyroid disease. However, you may be at increased risk for future thyroid disease, and your doctor may want to monitor your condition. For unknown reasons, the risk tends to be higher in women.
Calcitonin; The calcitonin test is primarily used to help diagnose C-cell hyperplasia and medullary thyroid cancer, to evaluate the effectiveness of treatment, and to monitor those affected for recurrence. It is also ordered to screen for medullary thyroid cancer in family members of people with multiple endocrine neoplasia type 2 (MEN 2). C-cell hyperplasia and medullary thyroid cancer are two rare conditions in which excessive amounts of calcitonin are produced. C-cell hyperplasia is a benign condition that may or may not progress to become medullary thyroid cancer.
A low level of calcitonin means that it is unlikely that symptoms are due to C-cell hyperplasia or medullary thyroid cancer. An elevated concentration of calcitonin means that excessive amounts are being produced. Significantly elevated levels of calcitonin are a good indicator of C-cell hyperplasia or medullary thyroid cancer; however, the healthcare practitioner will use other procedures, such as a thyroid , scan, biopsy and ultrasound, to establish the diagnosis.
With successful treatment for medullary thyroid cancer, which may involve removal of the thyroid gland and often some surrounding tissues, calcitonin levels will usually fall to very low levels. If the values stay low over time, then it is likely that the treatment was effective. In some cases, calcitonin levels will fall but remain moderately elevated after treatment. This means that some calcitonin-producing tissue remains. Healthcare practitioners will monitor calcitonin and watch for increases over time. If calcitonin levels begin to rise, then it is likely that there is a recurrence of medullary thyroid cancer.
With medullary thyroid cancer and C-cell hyperplasia, other thyroid tests, such as T4, T3, and TSH, are usually normal while calcitonin levels are elevated.
Calcitonin levels may also be elevated with lung, breast, and pancreatic cancers, insulinomas (tumor in the pancreas that produces too much insulin), and rare pancreatic tumors called VIPomas (cancer that usually grows from islet cells in the pancreas).
Concentrations of calcitonin may be increased with use of drugs such as epinephrine, glucagon, and oral contraceptives, and are normally higher in newborns as well as in women during pregnancy.
Other conditions with elevated calcitonin include: Intestinal, gastric, or bronchial carcinoid tumors, chronic renal failure, Zollinger-Ellison syndrome, and pernicious anemia.
rT3, reverse T3; is a competitive inhibitor to T3 and T4. Leptin resistance is directly correlated with reverse T3. Leptin is a hormone that controls all of energy metabolism in the body. It controls all the other hormones in the body as well. If it is not working well, the rest of your hormones are going to show clinical problems as well. Many people think they have thyroid issues when they actually have leptin resistant. One becomes leptin resistant when the brain no longer recognizes the leptin signal sent from our fat cells. Testing leptin is easy to do but rarely done in medicine today. Biochemically it can be done with thereverse T3 test. Leptin resistance completely turns off your thyroid gland making it so you cannot burn fat in your muscles because it down regulates your basal metabolic rate.
T3, free (Free Triiodothyronine) – measures the free, unbound levels of the hormone triiodothyronine – the active thyroid hormone at the cellular level. Because the free levels of T3 represent immediately available hormone, free T3 is thought to better reflect the patient’s hormonal status than total T3.
Elevated Free T3 – Elevated Free T3 may be indicative of hyperthyroidism.
Low Free T3 – Low Free T3 levels below the reference range may be indicative of hypothyroidism.
Optimal Free T3 – Some integrative physicians and hormone experts state that if free T3 is not in the top half – or even the top quarter – of the reference range, it is not optimal.
T4, free – measures the free, unbound thyroxine levels (the storage hormone), in your bloodstream. Free T4 is typically elevated in hyperthyroidism, and lowered in hypothyroidism. Free or unbound T4 levels represent the level of hormone available for uptake and use by cells. Because the free levels of T4 represent immediately available hormone, free T4 is thought to better reflect the patient’s hormonal status than total T4.
TSH, Thyroid-stimulating hormone is a hormone that stimulates the thyroid gland to produce T3 and T4. Releasing hormone from the hypothalamus causes the release of the hormone TSH from the anterior pituitary gland, which finally allows the release of the hormones T3 and T4 from the thyroid gland.
You could have a perfectly functioning thyroid; but if your pituitary gland is not sending over the correct TSH levels to your thyroid telling it to go to work… Then it doesn’t. If that is the case, you have a lack of T4 & T3 hormones being produced in your body; a condition known as “hypothyroidism”.
If your pituitary gland is constantly bombarding your thyroid with high TSH levels, it kicks the thyroid into overdrive, and your thyroid starts producing too much T3 & T4 hormones. This is what causes the condition known as “hyperthyroidism”.
When the thyroid does not produce enough thyroid hormones, the pituitary detects this reduction in thyroid hormones, and it tries to stimulate the thyroid into action by producing and sending over more TSH. This is the pituitary gland’s effort to return the TSH levels to “normal” and balance the thyroid’s function. Therefore, higher TSH levels than normal suggests a thyroid that is under-active and not doing its job of producing thyroid hormone. So, in general, higher levels of thyroid stimulating hormone equals an under-active thyroid; or hypothyroidism.
And the opposite is true. If the thyroid is overactive and producing too much thyroid hormone, the pituitary senses that there is a thyroid hormone overload circulating through the system.
The pituitary then usually slows or shuts down thyroid stimulation, so that the thyroid will slow down its production of the T3 & T4 hormones. This drop in TSH is the pituitary gland’s attempt to return circulating T3 & T4 hormone levels to normal. Therefore, the TSH test results will show lower than normal TSH when the thyroid is overactive. So, in general, lower TSH levels equals an overactive thyroid; or hyperthyroidism.